Study on the Assessment of Clinical & Neuroimaging Features of Acute Encephalitis Syndrome & Their Prognostic Significance among Children Admitted in the Pediatric Emergency Ward of Burdwan Medical College, Burdwan
Original Article
Abstract:
Background & Objectives: Acute encephalitis syndrome (AES) is a major cause of morbidity & mortality in India. Studies regarding clinical & imaging features of AES & their prognostic significance are rare. Hence this study was conducted to identify clinical & radiological features of AES &prognostic significance of them.
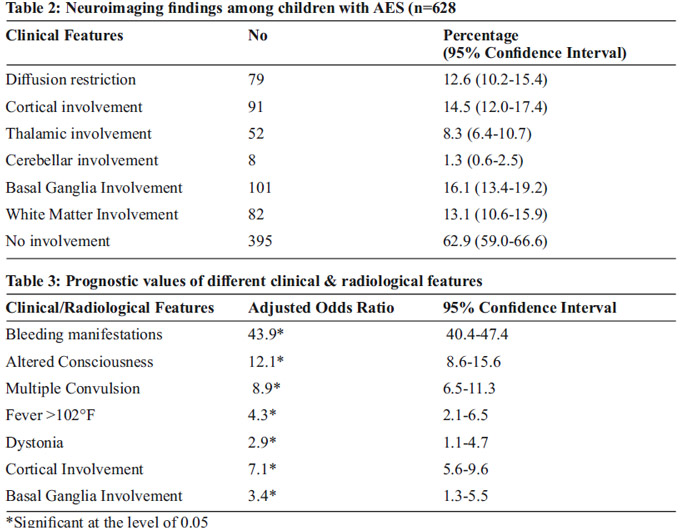
Methodology: Hospital based prospective study. 628 samples were selected by complete enumeration method. Data were collected by using a pre-tested pre-designed semi-structured schedule. Statistical analysis was done by SPSS version 19.0. P<0.05 was taken as statistically significant. Common radiological findings included basal ganglia involvement (16.1%), cortical involvement (14.5%), white matter involvement (13.1%) & diffusion restriction (12.6%). Cerebellar involvement was least common (1.3%).
Results: Mean age of the study population is 5.3±2.1 years & 62.1% of them were boys. Clinical features includes fever between 100-102° F (76.0%) & convulsions of <2 episodes (48.1%). altered consciousness (46.5%), cranial nerve palsy (16.2 %), motor weakness (11.3 %) & tone disturbance (19.7 %) & bleeding manifestations (9.7% ). Common radiological findings included basal ganglia involvement (16.1%), cortical involvement (14.5%), white matter involvement (13.1%) & diffusion restriction (12.6%). Cerebellar involvement was least common (1.3%). Bleeding manifestation was the worst prognostic indicator (Adjusted odds ratio-43.9).
Conclusion: Appropriate national program, vaccination & vector control can prevent disabilities & deaths from AES.
Keywords: Acute encephalitis syndrome, neuroimaging, Japanese encephalitis
Introduction:
Acute encephalitis syndrome (AES) is an important cause of mortality & morbidity among children affecting 6-10/100000 children & case fatality ratio varies between 20-50%.1,2 AES is mainly caused by neurotrophic viruses namely enterovirus, different types of arbovirus including Japanese encephalitis virus, chandipura virus, west nile virus, dengue virus etc. Apart from virus acute bacterial meningitis, tuberculous meningitis, toxoplasmosis, neurocysticercosis may also present as AES. Cause of AES is different depending on season & geographical location & mainly affects children below 15 years of age.3,4 Many species of mosquitoes act as carrier of vectors and cattles served as amplifier hosts of these deadly viruses. Clinical features of AES are variable including fever, headache, convulsion, alteration of consciousness etc. Apart from causing considerable mortality, AES is an important cause of morbidity in forms of muscular weakness, convulsion disorders, speech/visual abnormality etc. History of AES in India can be divided into three phases, before 1975: few JE cases were identified, between 1975-1999: mainly JE cases were identified & after 1999 mainly non-JE outbreaks became predominant.5 After 2012, some outbreaks of JE is noted in India.6,7 There are few studies regarding clinical presentation of AES in Indian settings. To the best of our knowledge no studies are conducted in India regarding the radiological/ imaging findings of AES children. Few studies were carried out regarding prognostic of different clinical/imaging findings of tuberculous meningitis/ bacterial meningitis/ Japanese encephalitis, but no study was found on the prognostic significance of different findings of AES.8,9 Hence this study was carried out in the Pediatric in-patient department of Burdwan Medical College to find the clinical & radiological features of AES along with their prognostic significance.
Methods:
One hospital (in-patient)-based prospective study was conducted among children (<12 years) admitted with features of AES in the Pediatric Emergency Ward of Burdwan Medical College, a rural tertiary care centre in between January, 2015 to December, 2017. All patient admitted with AES in the specified time period were selected for the study & complete enumeration methods is thus followed. Children who were previously diagnosed as neurological diseases, who were seriously ill to undergo a neuroimaging procedure or whose parents were not willing to give consent were excluded from the study. 642 children were admitted with a clinical diagnosis of AES in the study period & 14 children were excluded from the study (2 for not giving consent, 4 children were previously diagnosed as static encephalopathy & 8 children were died before any neuro-imaging procedure). So, the study population came to be 628. Data were collected by using a pre-designed pre-tested semi-structured schedule. Physical examination was done by same investigator in all cases which is confirmed by other investigators. Every CT/MRI plates were checked by two different radiologists. Prior ethical clearance was taken. [BMC/PG/194/1(1)]
Operational Definition:
AES was defined as “Acute onset of fever for not more than 5-7 days duration associated with changes in mental status with/without new onset seizure (except febrile seizure) irritability, somnolence, behavioral abnormalities.”10
Statistical Analysis:
Collected data were entered into Microsoft Office Excel Worksheet after double-checking. Continuous data were expressed in the terms of mean & standard deviation, whereas proportions were used for categorical variable. Spearman’s rank order correlation coefficient (ρ) was used for assessment of degree & direction of association. A binary logistic regression model was used to calculate adjusted odds ratio with 95% confidence interval using death as the outcome variable (Death=1, Discharged/disabled=0).All the analysis was done by SPSS version 19.0 (Statistical package for social sciences). All the data were rounded to one decimal point. P<0.05 was taken as statistically significant.
Results:
Mean age of the study population was 5.3±2.1 years. Among them 62.1% were boys & 70.4% were from rural population. Majority of them belonged to lower socioeconomic status according do modified BG Prasad scale. Among 628 children admitted with AES, 439 (69.9%) were successfully discharged. 17.5% developed disability & 79 (12.5%) of them were expired.
Majority of them presented with fever between 100°F-102°F (76.0%) & convulsion of <2 episodes (48.1%). Altered level of consciousness was found among 46.5% patients. Majority of them presented with confusion/delirium (15.8%) followed by obtundation (8.8%). Cranial nerve palsy was found among 16.2 % children, among them facial nerve palsy was most common (86.1%). Motor weakness was present among 11.3 % of study population, paraparesis being most common (59.2%). Tone disturbance was noted among 19.7 % children with AES & dystonia was most common clinical finding among them. Bleeding manifestation is noted among 9.7% children [Table 1]
No significant radiological findings were noted among 62.9% of children affected with AES. Common radiological findings were basal ganglia involvement (16.1%), cortical involvement (14.5%), white matter involvement (13.1%) & diffusion restriction (12.6%). Cerebellar involvement was least common (1.3%). [Table 2]
It was noted that bleeding manifestation (ρ=0.0.83), fever >102°F (ρ=0.47), altered state of consciousness (ρ=0.82), convulsion (ρ=0.79), tone disturbances (ρ=0.41), motor weakness (ρ=0.39), cranial nerve palsy (ρ=0.28), cortical involvement (ρ=0.68), basal ganglia involvement (ρ=0.59) & diffusion restriction (ρ=0.50) were significantly & positively correlated with adverse outcome i.e. death. Among them, bleeding manifestation had the strongest correlation with the adverse outcome.
These variables were further considered for binary logistic regression, stepwise method for calculation of adjusted odds ratio with 95% confidence interval. Bleeding manifestation was the most dangerous risk factor associated with adverse outcome (Adjusted odds ratio-43.9). Patients who developed altered consciousness, multiple convulsions, fever>102°F & dystonia were 12.1, 8.9, 4.3 & 2.9 times more prone to experience the adverse outcome. Among the imaging features, cortical involvement & basal ganglia involvement were emerged out as significant having an adjusted odds ratio of 7.1 & 3.4 respectively.
Discussion:
In our study we found that AES mainly affected boys from rural population & lower socioeconomic status. Clinical findings were fever, convulsion, alteration of sensorium, tone disturbances, cranial palsy, motor weakness & bleeding manifestations. Imagning findings include involvement of cortex, basal ganglia, white matter & cerebellum in form of diffusion restriction/infarct etc. Bleeding manifestation emerged out as worst prognostic factor.
In our study mortality due to AES is 12.5% which is comparable to the findings of Burke DS et al & Maha MS et al.11,12 However, it is higher than that of the developed countries.13 Rao BL et al 7 & Gurav YK14 et al also reported the similar type of presentations of AES from different part of country.
Presence of seizure, fever, tone disturbances & alteration of sensorium was described as poor prognostic factors by many authors. Similarly we also noted that they are associated with adverse outcome.15,16 Huy BV et al noted that need of assisted/mechanical ventilation is a bad prognostic factor.17 But we do not found it as a prognostic marker. But they considered disability as an adverse outcome too, we only considered death as an adverse outcome. Similar bad prognostic factors were also found by different authors in Indian settings for tuberculous & pyogenic meningitis.8, 9
Conclusion:
Though the sample size is adequate according to statistics, this study may reflect findings of a rural population. So findings of the present study may not be generalizable. Further studies especially multi-centric studies should be conducted.
AES is a major cause of morbidity & mortality in India. Proper treatment guidelines may result in a decrease in morbidity & mortality. Appropriate national Health Program on AES, especially vector control is needed for further betterment. JE can be prevented by vaccination. Proper advertisement in mass-media may be helpful.
Contibution:
MKG- Revising manuscript, Checking MRI/CT plates, KI-Collection & analysis of data, writing manuscript, AKD- Revising manuscript, concept of study, AR- Revising manuscript, RDCollection of data, SS-Collection of data.
Conflict of Interest: None
Source of Funding: Nil
Common radiological findinds are in Basal Ganglia , Cortex and white matter.Cerebellar Involvement is Least.
Bleeding Manifestation was the Worst Prognostic Indicator.
References:
1. Solomon T, Thao TT, Lewthwaite P, Ooi MH, Kneen R, Dung NM, et al. A cohort study to assess the new WHO Japanese encephalitis surveillance standards. Bulletin of the World Health Organization 2008;86:178–86.
2. Jmor F, Emsley HC, Fischer M, Solomon T, Lewthwaite P. The incidence of acute encephalitis syndrome in Western industrialised and tropical countries. Virology Journal 2008;5:134
3. Kar NJ, Saxena VK. Some epidemiological characteristics of Japanese encephalitis in Haryana state of northern India. Journal of Communicable Diseases 1998;30:129–31
4. Sapkal GN, Bondre VP, Fulmali PV, Patil P, Gopalkrishna V, Dadhania V, et al. Enteroviruses in patients with acute encephalitis, Uttar Pradesh, India. Emerging Infectious Diseases 2009;15:295–8
5. Joshi R, Kalantri SP, Reingold A, Colford JM., Jr Changing landscape of acute encephalitis syndrome in India: a systematic review. Natl Med J India. 2012;25:212–220.
6. Chadha MS, Arankalle VA, Jadi RS, Joshi MV, Thakare JP, Mahadev PV, et al. An outbreak of Chandipura virus encephalitis in the eastern districts of Gujarat state, India. American Journal of Tropical Medicine and Hygiene 2005;73:566–70.
7. Rao BL, Basu A, Wairagkar NS, Gore MM, Arankalle VA, Thakare JP, et al. A large outbreak of acute encephalitis with high fatality rate in children in Andhra Pradesh, India, in 2003, associated with Chandipura virus. Lancet 2004;364:869–74.
8. Kalita J, Misra UK. Outcome of tuberculous meningitis at 6 and 12 months: a multiple regression analysis. International Journal of Tuberculosis and Lung Disease 1999; 3:261–5.
9. Singhi P, Bansal A, Geeta P, Singhi S. Predictors of long term neurological outcome in bacterial meningitis. Indian Journal of Pediatrics 2007;74:369–74.
10. Guidelines: clinical manifestations of acute encephalitis syndrome including Japanese encephalitis: Government of India. p 1.Aug,2009.
11. Burke DS, Lorsomrudee W, Leake CJ, Hoke CH, Nisalak A, Chongswasdi V, et al. Fatal outcome in Japanese encephalitis. American Journal of Tropical Medicine and Hygiene 1985;34:1203–10.
12. Maha MS, Moniaga VA, Hills SL, Widjaya A, Sasmito A, Hariati R, et al. Outcome and extent of disability following Japanese encephalitis in Indonesian children. International Journal of Infectious Diseases 2009
13. Kennedy CR, Duffy SW, Smith R, Robinson RO. Clinical predictors of outcome in encephalitis. Archives of Disease in Childhood 1987;62:1156–62
14. Gurav YK, Bondre VP, Tandale BV, Damle RG, Mallick S, Ghosh US, Nag SS. A large outbreak of Japanese encephalitis predominantly among adults in northern region of West Bengal, India. J Med Virol. 2016 Nov;88(11):2004-11
15. Kennedy CR, Duffy SW, Smith R, Robinson RO. Clinical predictors of outcome in encephalitis. Archives of Disease in Childhood 1987;62:1156–62.
16. Bhutto E, Naim M, Ehtesham M, Rehman M, Siddique MA, Jehan I. Prognostic indicators of childhood acute viral encephalitis. Journal of Pakistan Medical Association 1999; 49:311–6
17. Huy BV, Tu HC, Luan TV, Lindqvist R. Early mental and neurological sequelae after Japanese B encephalitis. Southeast Asian Journal of Tropical Medicine and Public Health 1994;25:549–53
Issue: January-March 2018 [Volume 7.1]