Risk Stratification and Care Plan for Intervention using Indian Academy of Pediatrics Malnutrition Proactive Assessment – A Comprehensive Tool (IMPACT) among Under-five Children with Varying Ailments
Original Research
Abstract:
Objective: To evaluate the quality of life (Q) and plan for intervention, IAP proposed a tool ‘IMPACT’ (IAP’s Malnutrition Proactive Assessment-A Comprehensive Tool). [10] The study was aimed to implement, assess and evaluate the ease of use of the proposed IMPACT tool in a busy OPD so as to derive an intervention plan for improving quality of life depending on the estimated risk level.1.To implement and assess the utility of IMPACT. 2.To evaluate its ease of use in a busy pediatric OPD setup.
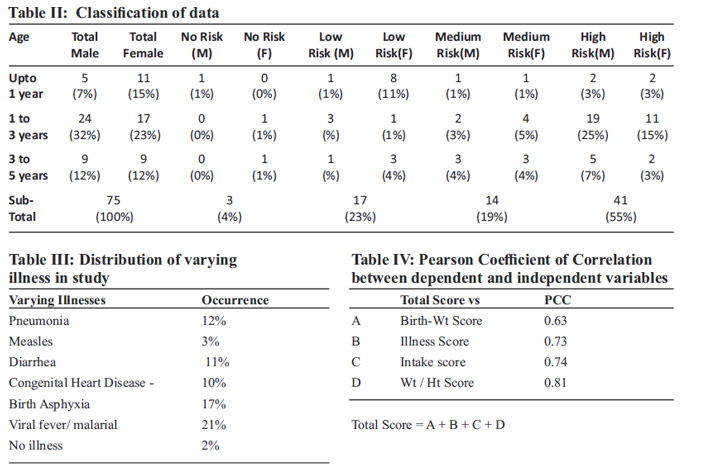
Methods: A retrospective study was carried out on data of 75 children aged between 0.5 to 5 years. Using IMPACT criteria, scores were assigned to each 4 recorded parameters. Risk stratification was determined from the Total Score for each child. Pearson correlation coefficient (PCC) was calculated in MS Excel for each of the independent variables vs the dependent variable.
Results: Out of 75 children IMPACT indicated that 55%, 19%, 23% and 4% were at High, Medium, Low and No risk respectively. 73% of the children at High risk, were in the 1-3 years age group. Best values of PCC was 0.81 with Weight/Height. Where the Weight/Height percentile score were 0 (there is no wasting or already corrected), the total IMPACT score identified 45% more children at medium or high risk level.
Conclusion:IMPACT tool provides a robust and efficient method of detecting malnutrition risk level in children.
KEY WORDS: ABCDEF Assessment, Weight/ height, Indian Academy of Pediatrics Malnutrition Proactive Assessment – A Comprehensive Tool (IMPACT), Quality of life
Introduction
Major causes accounted for under 5 mortality rate are birth asphyxia, preterm, pneumonia, diarrhea and malaria. About 45% of all child deaths are linked to malnutrition. [1] According to recently released National Family Health Survey(NHFS), nearly every third child under five years is undernourished—underweight (35.7%) or stunted (38.4%) and (21%) are wasted in India. [2] This clearly shows that the onset of malnutrition in Indian children occur very early. ICP (Infant Child and Puberty) model by Karlberg showed that nutrition is most important determinant of all 3 components of model for normal growth and development [3].The consequences of malnutrition are diverse. It not only affects mortality and morbidity by having a negative effect on multiple organ functions, but also impairs intellectual and behavior development. These effects cannot be reversed. Quality of life encompass life satisfaction and both physical and mental well-being. Hence health care delivery should mainly focus on providing a high-quality of life. [4, 5, 6,] Prevalent practice of assessment of nutritional status consisted of ABCDEF: Anthropometry assessment, Biochemical indicators of malnutrition, Clinical assessment, Dietary assessment, Epidemiological / ecological evaluation, Functional evaluation. [7] Some of the limitations of this approach included inter and intra-observer reliability, [8,9] invasive procedures for biochemical and functional assessment indicators, time-consuming dietary assessment, long questionnaire. As part of NEP (Nutritional Educational Program) India under the guidance of IAP 2015, a holistic ‘ABCDEFQ assessment scale is recommended. To evaluate the quality of life (Q) and plan for intervention, IAP proposed a tool ‘IMPACT’ (IAP’s Malnutrition Proactive Assessment-A Comprehensive Tool). [10] The study was aimed to implement, assess and evaluate the ease of use of the proposed IMPACT tool in a busy OPD so as to derive an intervention plan for improving quality of life depending on the estimated risk level.
Material & Methods
A retrospective observational study was carried out among 75 children from 0.5 to 5 years old who attended the pediatric camps. These children were divided in 3 age groups from 0.5 to 1 year, 1—3 years and 3 to 5 years age. Underweight an indicator of malnutrition was interpreted as low wt for age and was taken as an entry to the present study. [11] According to the proposed Comprehensive Tool shown in Table I, all 4 parameters including (a) birth weight, (b) underlying condition affecting nutritional status (c) current nutritional intake and (d) weight for height percentile of the participants were recorded. Based on the scoring method provided by the tool, all the children were graded on each of independent parameters. Risk stratification was determined on the basis of the total score for each child. The intervention plan was derived in accordance with the risk level provided by the tool. Pearson coefficient of correlation (PCC) was calculated between Total score (dependent variable) and each of the independent parameters. Though weight for age was not an input parameter in tool for grading score, Pearson coefficient of correlation was also derived for wt/age with total score. Statistical analysis was performed using MS Excel.
Results
Out of 75 children 50.7% and 49.3% were male and female respectively. IMPACT indicated that 55%, 19%, 23% and 4% were at High, Medium, Low and No risk respectively. Of the children at High risk, 10%, 73%, 17% were in the age groups 0.5-1, 1-3 and 3-5 years respectively. Highest incidence of children at high risk found in 1-3 years age group corroborates with NHFS finding [2]. Male children were at higher risk than female children (Table II). Of all the children studied, 73% suffered from varying illnesses listed in Table III. The PCC was 0.63, 0.73, 0.74 and 0.81 respectively for birth weight score, current illness score, current nutritional take score, Wt/Ht score vs total score as shown in Table IV. The best correlation was seen with Wt/Ht (0.81). This shows a good correlation between total score and each of the 4 parameters. The variation in the PCC could be because of the subjectivity in the measurement of the input parameters.
Discussion
As seen in Figure 1, 45% children had a Wt/Ht percentile score of 0, yet the IMPACT score graded these children at medium or high risk level. Of these 29% were due to higher Intake score where as 41% were due to higher underlying illness score. This shows that using 4 points scoring method brings out more number of suspects than a single point scoring method. Most of the children visit doctors for their current illness and not for improper growth and development. Our observation justifies short-listing children with poor scores of weight for age then subjecting them to IMPACT score for risk level categorization. By early diagnosis and care, not only will abnormal Weight/Height, if present, get corrected, but also prevent these children from falling back into the pitch of malnutrition and developing an abnormal behavior also referred to as non-goal behavior. Various malnutrition assessment tools are available for children. [12,13] Unlike the IMPACT tool, none of these are as comprehensive or holistic in approach. Due to its comprehensive nature, IMPACT can and should be easily used by medical health worker, paramedical and community volunteers. Purpose of using this tool was accomplished as it identified individuals at risk of becoming malnourished and those who were already malnourished. Nutritional status in general was indicated but did not identify specific nutritional deficiencies. This new scoring system IMPACT aims to make the assessment easy, simple, quick, non-invasive and objective through a holistic approach. Proper plan for intervention in childhood malnutrition will definitely show improvement in interactive process of child’s communication and overall psychological wellbeing of child which is the need of the hour. Malnutrition includes both under-nutrition and over-nutrition, though the latter is not evaluated in detail by IMPACT. These have been addressed by the ‘ELIZ Modified IMPACT’ tool which is not in the scope of this study. [14] There is a need for more study of the IMPACT tool. Since this study was a cross-sectional retrospective analysis of available data, a longitudinal cohort study involving undernutrition and over-nutrition over a larger population is being planned.
Conclusion
IMPACT tool provides a robust and efficient method of detecting malnutrition risk stratification in children. Such a holistic approach is rewarding in preparing an optimum care plan of children.
Contributors:
Anjali Otiv was involved in data collection, interpretation, analyzing and drafting the article, KE Elizabeth conceived the study and revised the manuscript for intellectual content.
Conflict of Interest: None
Funding source and its role in the study: None
Malnutrition risk stratification is important at busy government setup in children. Such a holistic approach is rewarding in preparing an optimum care plan of children.
References.
1. WHO Children: reducing mortality. Available from:http://www.who.int/mediacentre/factsh eets/fs178/en/ .Accessed September 2016
2. NFHS-4 (20016-17). The Demographic Health Survey Programs. Available from: http://www.DHSprogram.com. Accessed 7TH September 2017.
3. Elizabeth KE. Normal Growth and Assesssment. In: Elizabeth KE, editor. Nutrition and Child Development: 5th edition, Paras Medical Publisher; Hyderabad 2015; 86-87.
4. Gabr M: Undernutrition and quality of life, World Rev Nutr Diet 1987, 49:1-21.
5. Rasheed S, Woods RT: Malnutrition and quality of life in older people: a systematic review and meta-analysis, Ageing Res Rev 2013, Mar;12(2):561-6.
6. Vetta F, Ronzoni S, Taglieri G, Bollea MR:The impact of malnutrition on the quality of life in the elderly, Clin Nutr 1999, Oct;18(5):259-67.
7. Elizabeth KE. Protein energy malnutrition (PEM) and severe acute malnutrition (SAM); In: Elizabeth KE, editor. Nutrition and Child Development: 5th edition, Paras Medical Publisher; Hyderabad 2015.;186-241
8. Stomfai S, Ahrens W, Bammann K, Kovács E, Mårild S, Michels N, et al . Intra- and inter observer reliability in anthropometric measure ments in children, Int J Obes (Lond) 2011, Apr;35 Suppl 1:S45-51.
9. Maryline Sicotte, Maria-Victoria Zunzunegui, Marielle Ledoux, Souleymane Ag Aboub – acrine, Vinh-Kim Nguyen, and the ATARAO group. Reliability of anthropo -metric measures in a longitudinal cohort of patients initiating ART in West Africa, BMC Medical Research Methodology 2010, 10:102.
10. Elizabeth KE: Crusade Against Malnutrition Nutritional Educational Program, Indian Pediatrics 2015, March; Vol 53: 203-205 .
11. Paul V, Lodha R, Agarwala A. Nutrition; In: Paul V, Bagga A, editors. GHAI Essential Pediatrics: 8th edition, CBS Publishers and Distributors Pvt Ltd; New Delhi 2013 .p.95.
12. Thomas PC, Marino LV, Williams SA, Beattie RM: Outcome of nutritional screening in the acute paediatric setting, Arch Dis child 2016, Dec;101(12):1119-1124.
13. White M, Lawson K, Ramsey R, Soh XY , Dennis N, Hutchinson Z et al. Simple Nutrition Screening Tool for Pediatric Inpatients, JPEN J Parenter Enteral Nutr 2016, Mar;40(3):392-8.
14. Elizabeth KE: ELIZ Modified IMPACT’ – A Tool for Under Nutrition & Obesity- The Dual Burden of Malnutrition, BAOJ Pediat 2017, 3: 1 -3: 033.
Issue: January-March 2018 [Volume 7.1]