Filariasis Presenting as Puo With Renal and Hematological Abnormalities
Case Report
The Filarial worms Brugia malayi (Malayan Filariasis), Brugia timori, and Wuchereria bancrofti (bancroftian Filariasis) are threadlike nematodes that cause similar infections. Infective larvae are introduced into humans during blood feeding by the mosquito vector. The clinical manifestations of B. malayi, B. timori, and W. bancrofti infection are similar; manifestations of acute infection includetransient, recurrent lymphadenitis and lymphangitis. The early signs and symptoms include episodic fever, lymphangitis of an extremity, lymphadenitis (especially the inguinal and axillary areas), headaches, and myalgias that last a few days to several weeks.We reported uncommon presentation like acute kidney failure.
Case Report
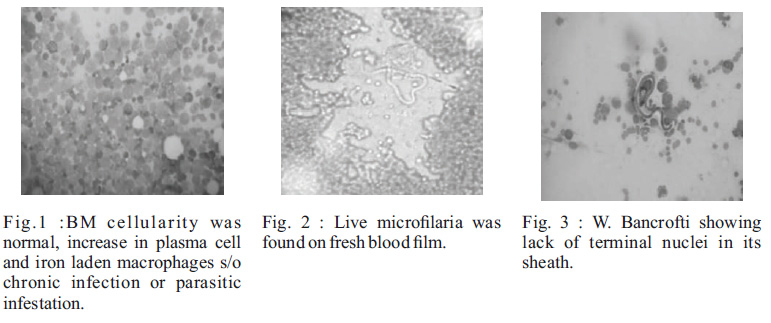
A 12 years old female patient residing in kharghar slum area presented with complaints of fever since 4 days, vomiting & abdominal pain since 2 days.She had not passed urine since last 18 hours. No other signi??cant history of medical and surgical symptoms. There was no signi??cant past history. On examination child was febrile and her eart rate and respiratory rate werw106/min and 28/min respectively with blood pressure being 90/50 mmHg. There was no lymphadenopathy or organomegaly. In view of the above complaints child was investigated. Routine complete blood picture showed Hb-8.8 mg/dl, TLC – 9900 (P82/L17/E1), platelet -86000 cells/mm3, M C V- 9 0 . 8 . D i m o r p h i c a n e m i a w i t h thrpmbocytopenia seen on peripheral smear. Urine R & M showed proteinuria(2+) and microscopic haematuria(3+). Her BUN was 71.3 and Creatinine was 4.1. Retic count was 2 with corrected retic count 1.1. Her ESR was 110. Till now this all clinical, pathological and biochemical reports suggestive of renal and hematological system involvement. Child had high creatinine value of 4.11, sodium 136 and potassium of 4.9 so her urine output was monitored and found to be oliguric. USG abdomen done was s/o medical renal disease. Work up for fever like Dengue NS1ag, RMA, PSMP, Typhi DotM were negative. Stool routine & occult blood was normal.The provisional diagnosis was Acute kidney injury (?HUS) due to infectious cause was thought of . Child was shifted to PICU. Fluid challenge was given followed by fuid and Lasix was given and restricted fuids started.Child gradually started improving in terms of urine output and serum creatinine value.Child was Shifted to ward after 48 hours. However Child started having continuous fever again. Her Hb dropped down from 8.8 to 6.4mg%. WBC count has increased from 9900 to 24200, platelet count droped from 86000 to 60000. Blood culture was sterile after 48 hours. Because obvious common etiology was not found on these routine investigations and child had involvement of renal and hematological systems with fever so bone marrow was done on 6th day of admission. In BM cellularity was normal, increase in plasma cell and iron laden macrophages suggestive of chronic infection or parasitic infestation (Figure 1). Eosinophil count was 15%. One live micro??laria was detected in fresh blood ??lm(Figure -2). A peripheral smear sent at 12 am showed microcytic hypochromic anaemia, thrombocytopenia, and live micro??laria of Wucheria Bancrofti as it lacked terminal nuclei(Figure -3). A diagnosis of microcytic hypochromic anaemia with W.bancrofti ??lariasis was made and child started on DEC, vitamin B12 and Folic acid.Family screening with help of mid night smear was done and parents and one sibling was found positive for Wucheria Bancrofti (only one sibling was not found positive). Retrospectively when inquired family has migrated from Bihar one year ago and surprisingly till now, all are asymptomatic. All family members were treated with DEC for 21 days and repeat mid night smear after 21 days done which were negative.
Discussion
* Lymphatic flariasis caused by Wuchereria bancrofti and Brugia malayi is an important public health problem in India. The most widespread LF infection is due to W. bancrofti (98%) and the remaining infection by B.malayi (2%) [1]. Filariasis is endemic in 17 States and 6 Union Territories, with about 553 million people at risk of infection.[1] . Humans act as a de??nitive host and mosquitoes are the intermediate host. The larvae enter through the skin, reach lymphatic channels and settle down in the lymph nodes. They mature and produce new larvae in 15-18 months. These then enter through the thoracic duct into the venous system and ??nally into the peripheral circulation. While circulating, these get lodged into a variety of organs and are picked up in Fine Needle Aspiration smears from the thyroid, breast, subcutaneous nodules or other organs, or in tissue samples such as bronchial washings.[2-7]. Their ability to cross the vessel wall allows them to settle in the bone marrow also. In our patient, Filariasis was not suspected clinically due to the lack of a typical clinical picture. Bone marrow aspirate was done to evaluate pyrexia of unknown origin and bicytopenia, revealed ??nding of micro??laria. This ??nding prompted the collection of a midnight blood sample and the subsequent ??nding of micro??laria in the peripheral smear. Our case was unique in having bicytopaenia with raised Total Leukocyte Count along with features of acute renal failure , treated successfully with DCE and cured after treatment. According to a study conducted by J. Langhammer et al. [8], renal failure can occur due to tubular damage, even in asymptomatic micro??laraemia[8]. In symptomatic patients, there is glomerular damage occurring as a result of circulating immune complexes, which usually manifests as proteinuria and/or haematuria.[9]. A.D. Omerod found Immune complex glomerulonephritis and chronic anaerobic urinary infection–complications of filariasis.[10]
References
1. Lymphatic filariasis in India Epidemiology and control measures Sabesan S, Vanamail P, Raju K, Jambulingam P – J Postgrad Med.
2. Yenkeshwar PN, Kumbhalkar DT, Bobhate SK. Micro??lariae in ??ne needle aspirates: a report of 22 cases. Indian J Pathol Microbiol 2006;49:365-69.
3. Kishore B, Khare P, Gupta RJ, Bisht SP. The micro??lariae of Wuchere- ria bancrofti in cytologic smears: a report of 5 cases with unusual presentations. Acta Cytol 2008;52:710-12.
4. Gupta S, Gupta R, Bansal B, Singh S, Gupta K, Kudesia M. The signi??cance of the incidental detection of filariasis on aspira tion smears: a case series. Diagn Cytopathol 2010;38:517-20.
5. Anupindi L, Sahoo R, Rao RV, Verghese G, Rao PV. Micro??lariae in the bronchial brushing cytology of symptomatic pulmonary lesions. A report of two cases. Acta Cytol 1993;37:397-99.
6. Srikanth S. Micro?? laria in thyroid aspirate- An unusual finding. Thyroid Research and Practice | January-April 2014 | Vol 11 | Issue 1:26-8.
7. Col R Ravikumar,Col KK Sen, Surg Lt Cdr SN Singh,Surg Capt N Chawla, SR Choudhary,Maj D Singh. Filarial Dance in a Breast LumpMJAFI 2010; 66 : 193-195
8. J. Langharnrner, H. -W. Birkl and H. ??ahner Renal disease in lymphatic filariasis: evidence for tubular and glomerular disorders at various stages of the infection. Tropical Medicine and International Health Volume ?? NO 9 PP 875- 884 September1997.
9. Dreyer G., Ottesen E.A., Galdino E., Andrade L., Rocha A.,Medeiros Z., Moura I., Casimiro I.,Beliz F., Coutinho A. (1992) Renal abnormalities in microfilaremic patients with Bancroftian filariasis. Am. J. Trop. Med. Hyg. 46:745–751
10. A.D.Ormerod- Postgrad Med J 1983;59:730- 733 doi:10.1136/pgmj.59.697.730
Issue: July-September 2015 [Volume 4.3]
