Etiology, risk factors and morbidity profile associated with neonatal hyper bilirubinemia in a tertiary care hospital
Original Research
Abstract:
Hyperbilirubinemia is one of the most common and one of the most vexing problems that occur in the neonate1. Most adults are jaundiced when serum bilirubin levels exceeds 2mg%. Neonates, however may not appear jaundiced until the serum bilirubin concentration exceeds 5 to 7 mg%2.
Aims And Objectives:
- To study common causes and risk factors of neonatal hyperbilirubinemia.
- To study immediate morbidity associated with neonatal hyperbilirubinemia
- To study mortality profile associated with neonatal hyperbilirubinemia.
Material And Methods:
The present study was conducted at Department of Pediatrics of Shree Vasantrao Naik Govt. Medical College and hospital, Yavatmal from, June 09 to May10.
Results:
120 neonates were studied, of which 68 were male and 52 were females. Out of 120 neonates, 49neonates were less than 37 weeks gestation and 71 neonates were having gestational age more than 37 weeks. Out of 49 neonates with gestational age less than 37 weeks 21 (42.85%) were between 28- 30 weeks gestation, 20 (40.81%) were between 30- 32 weeks gestation and 08 (16.33%) neonates had gestational age between 33-36 weeks.
Keywords:
Neonatal hyperbilirubinemia, neonatal jaundice, Gestational age, Prematurity.
Introduction:
Hyperbilirubinemia is one of the most common and one of the most vexing problems that occur in the neonate1. Most adults are jaundiced when serum bilirubin levels exceeds 2mg%.Neonates, however may not appear jaundiced until the serum bilirubin concentration exceeds 5 to 7 mg%2.
Jaundice is the commonest abnormal physical finding in the neonates3.The overall incidence of neonatal jaundice as reported by various Indian workers varies from 54.6% to 77% 4. Jaundice occurs when the liver cannot clear a sufficient amount of bilirubin from the plasma.5 Yellowish discoloration of the skin is the result of accumulation of unconjugated non-polar lipid soluble indirect reacting bile pigment.6
Pathological jaundice is known to occur in 4- 8%of newborn babies. The common causes include blood group incompatibilities, prematurity, sepsis, G6PD deficiency and majority being idiopathic. Other less common causes include polycythemia, cephalhematoma7, 8. Immature newborn brain is susceptible to toxicity from unconjugated bilirubin resulting in “Kernicterus” or “bilirubin induced brain damage” (BIND).9
Assessment of jaundice should be done in the natural light. The pulp of finger or thumb is pressed on baby’s skin, preferably, over a bony part till it blanches and underlying skin is noted for yellow colour.
The criteria for intervention to control hyperbilirubinemia vary in different clinical situations. Phototherapy is a cheap, effective and safe method of management of neonatal hyperbilirubinemia. It is effective in treating hemolytic as well as non-hemolytic hyperbilirubinemia. Prophylactic phototherapy is indicated for infants weighing less than 1500 grams (serum bilirubin level less than 5 mg %).10,11
The present study will further try to analyze causes and risk factors related to neonatal hyperbilirubinemia and will also study relationship of hyperbilirubinemia with gestational age, birth weight and maternal risk factors along with response of such cases to the treatment.
Aims And Objectives:
- To study common causes of neonatal hyperbilirubinemia.
- To study risk factors for neonatal hyperbilirubinemia.
- To study immediate morbidity associated with neonatal hyperbilirubinemia.
- To study mortality profile associated with neonatal hyperbilirubinemia
Material And Methods:
The present study was conducted at Department of Pediatrics of Shree Vasantrao Naik Govt. Medical College and hospital, Yavatmal from, June 09 to May10.
Selection of cases:
The babies delivered at the hospital as well as babies referred from peripheries of age between 0- 28 days in 1 yr duration were included in this prospective study. All the neonates i.e. full term, preterm, healthy and sick neonates were included.
Sample size:
Comprised of 120 neonates with jaundice (those with serum bilirubin more than 10 mg/dl) hospitalised in pediatric units at V.N. Govt. Medical College and hospital during study period.
Sampling method:
A total of 120 hospitalised neonates satisfying selection criteria were recruited.
Inclusion criteria:
1)Neonates with jaundice delivered inside or outside the institute ,admitted in NICU and pediatric ward respectively at Government Medical College, Yavatmal during study period.2)Age group between 0-28 days.3)Neonates of either sex male/female.4)Those were willing to participate in the study.
Exclusion criteria:
- Babies attending outpatient department only.
- Babies who went discharge against medical advice.
- Babies who did not consent to participate in the study.
Method:
Jaundice was ascertained by clinical methods and was confirmed by biochemical methods. Each baby delivered at hospital was carefully observed from birth onwards in day light, for appearance of jaundice. In babies with dark complexion, digital pressure over fore head was used to detect the icterus.
In addition, babies coming from peripheries were examined thoroughly clinically and detailed investigations (given below) were done to detect the cause of jaundice using predesigned proforma.
Serum bilirubin estimation was done by Van den Bergh method. The babies who were having serum bilirubin 10 mg/dl or less were not included in the study. Only those having serum bilirubin more than 10 mg /dl were included in the study.
Detailed antenatal, natal and postnatal history was taken. Thorough clinical examination of every baby was done and all the necessary investigations for hyperbilirubinemia were carried out. Babies were treated according to need by phototherapy, drug therapy and exchange transfusion. Serum bilirubin levels were monitored from time to time. Newborns were treated according to standard guidelines and observed throughout their stay in hospital.

Out of 120 neonates, 49neonates were less than 37 weeks gestation and 71 neonates were having gestational age more than 37 weeks.
Out of 49 neonates with gestational age less than 37 weeks 21 (42.85%) were between 28-30 weeks gestation, 20 (40.81%) were between 31-32 weeks gestation and 08 (16.33%) neonates had gestational age between 33-36 weeks.

Out of 120 neonates, the aetiology was idiopathic hyperbilirubinemia in 42(35%) neonates, physiological hyperbilirubinemia seen in 36 (30%) neonates, ABO incompatibility was a cause of hyperbilirubinemia in 17(14.16%) neonates, septicemia in 10 (8.33%) neonates ,Rh incompatibility in 8 (6.66%) neonates, cephalhematoma in 3 (2.5%) neonates ,G-6-PD deficiency was a cause of hyperbilirubinemia in 1 (0.83) neonate ,and miscellaneous in 1 (0.83%) neonate, one neonate had both ABO incompatibility and septicemia, one neonate had both cephalhematoma as well as septicemia.

In the study of 120 neonates, 14(11.67%)neonates were between 1000gmto 1500 gm while 29(24.16%) neonates were between 1501 to 2000 gm. Maximum number of neonates i.e.37(30.84%) were between 2001 to 2500 gm,29 (24.16%)neonates were between 2501 to 3000 gm and 11(9.17%) neonates were above 3000 gm weight.
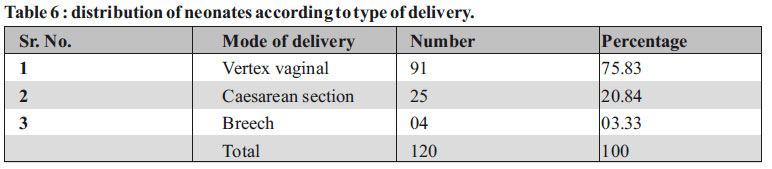
Out of 120 neonates, 91 (75.83%) neonates were born by vaginal delivery, 25(20.84%) neonates were born by Caesarean section and 4(3.33%) neonates were born by breech delivery.

In present study 38(31.67%) neonates were having serum bilirubin level between 11-15mg/dl, 46(38.33%) neonates had serum bilirubin between 15.1-18 mg%,21(17.50%) neonate’s serum bilirubin was between 18.1-20 mg/dl and in 15(12.5%) neonates it was more than 20mg/dl..

Two babies in this study developed bilirubin encephalopathy of which, one was premature baby with ABO incompatibility and other was term baby with Rh incompatibility who also had birth asphyxia.

As per above table 16 neonates required exchange transfusion with 3 neonates having Rh incompatibility,5 neonates having ABO incompatibility,5 neonates having idiopathic hyperbilirubinemia,2 neonates having septicemia and one neonate having G-6-PD deficiency.
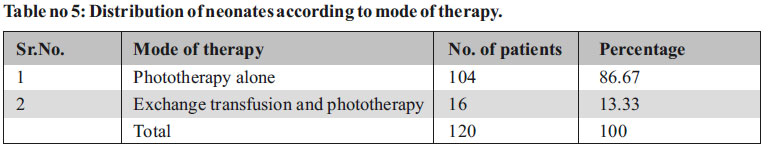
Of the total 120 neonates, 104 neonates were treated with phototherapy only and 16 neonates had to undergo exchange transfusion in spite of phototherapy.

As seen in table, the mean drop of bilirubin in Rh incompatibility after exchange transfusion was 12.9 mg/dl, in ABO incompatibility 11.5mg/dl, in septicemia 11.4mg/dl, in idiopathic hyperbilirubinemia 9 mg/dl and in a case of G-6-PD deficiency, it was 13.8 mg/dl.

As seen in the current table, the mean fall in bilirubin level after phototherapy was 5.6mg/dl in physiological hyperbilirubinemia, 6.4 mg/dl in idiopathic jaundice, mean decrease was 6 mg/dl in septicaemia, 6.9 mg/dl in ABO incompatibility, mean fall in bilirubin was 6.4 mg/dl in Rh incompatibility and 5.6 mg/dl in cephalhematoma.

During phototherapy 5 neonates developed loose motions and 4 neonates developed rash.
During exchange transfusion 1 neonate developed cardiac arrest and 3 neonates developed hypoglycemia. 2 neonates developed septicemia after exchange transfusion.
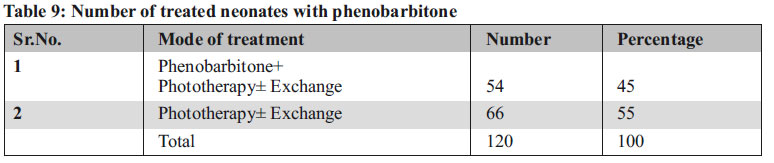
Out of 120 cases, 66 cases received phototherapy alone or along with exchange transfusion. In 54 cases, phenobarbitone was added along with exchange transfusion and phototherapy

In present study mean drop in bilirubin level was found to be 9.6mg/dl in the group, which received phenobarbitone as compared to 9 mg/dl in group which did not.
Maternal Factors:
As shown in above table, premature rupture of membrane was seen in 6 neonates of which 1 neonate had ABO incompatibility, 1 neonate had cephalhematoma, 1 had physiological hyperbilirubinemia and 3 neonates had septicemia.
Toxaemia of pregnancy was seen in 7 cases of which 1 had Rh incompatibility, 2 had idiopathic jaundice, 3 cases had physiological hyperbilirubinemia and 1 had septicemia.
Prolonged labour was seen in 11 cases of which,1 had ABO incompatibility,2 neonates had cephalhematoma,3 neonates had septicaemia and 5 neonates had idiopathic hyperbilirubinemia.
Oxytocin induction was done in 4 cases, out of which 3 had idiopathic hyperbilirubinemia and 1 neonate had cephalhematoma.
Fetal Factors:
Prematurity was aggravating factor in 26 neonates of which 3 neonates had ABO incompatibility,3 neonates had septicaemia,1 neonate had Rh incompatibility,18 neonates had physiological hyperbilirubinemia and 1 neonate had various congenital anomalies.
One premature baby had both ABO incompatibility and septicemia. One full term baby had both cephalhematoma and septicemia.
13 neonates had birth asphyxia of which 1 neonate had ABO incompatibility, 1 neonate had septicamia and 6 neonates had idiopathic jaundice and 5 neonates had physiological hyperbilirubinemia.
Discussion:
A total of 120 neonates of neonatal hyperbilirubinemia were studied in detail.
Sex Distribution:
Out of 120 neonates of hyperbilirubinemia 67% were males.
Narang et al12 have also found a male predominance in their studies with 56.2% cases of male sex.
Gestational Age:
49 neonates were having gestational age less than 37 weeks and 71 were of more than 37 weeks gestation. Out of 49 neonates, maximum cases were seen between the gestational age of 28-32 weeks with 21 neonates (42.86%) between 28-30 weeks, 20 neonates (40.82%) were between 31-32 weeks and 8 neonates (16.32%) were between 33- 36 weeks gestation.
Singhal et al13 have found prematurity as the second most common cause of hyperbilirubinemia in their studies. Prematurity was seen in 16.7% cases. Narang et al12 found jaundice in 440 (47.9%) out of 917 preterm babies.
Birth Weight:
In our study, maximum number (37) of neonates were having birth weight between 2001- 2500gm. 14 neonates (11.67%) were below 1500gm while 29 (24.16%) were between 1501 to 2000gm. 29 cases (24.16%) were between 2501- 3000gm and only 11 neonates (9.17%) had birth weight above 3 kg.
Most of the neonates i.e. 80 were less than 2.5 kg i.e. with low birth weight. Singhal et al13 found in his study that one fourth of neonates (29.16%) developing hyperbilirubinemia were with low birth weight.
Narang et al12 concluded from their studies that the incidence of neonatal jaundice was three times higher in LBW babies compared to babies above 2500 g.
In our study 66.66% neonates were low birth weight, it is mainly because of maternal under nutrition, poverty, under utilization of health services and illiteracy seen in this rural area.
Aetiology:
Physiological hyperbilirubinemia:
In 36 neonates, the jaundice was physiological as it appeared between 48-96 hours and disappeared by 6-7 days in term and 10-12 days in preterm infants. Peak serum bilirubin was seen on 4th day in term and 7th day in preterm babies.
In studies by Merchant R.H. 14, physiological jaundice was seen in 25.3% cases. Our ndings are close to their fndings.
Idiopathic hyperbilirubinemia:
In maximum number of neonates i.e 42 (35%) in our study, we were not able to find any cause and they were classified as idiopathic.
Merchant R.H. et al14 found idiopathic hyperbilirubinemia in 66% cases, Verma M. et al15 found idiopathic hyperbilirubinemia in 35% cases, Singhal et al13 found idiopathic hyperbilirubinemia in 34.4% cases while Narang et al12 found it in 57.8% cases. Our ndings are close to that of Verma et al15 and Singhal et al13.
Septicemia:
In 12 neonates septicemia was the cause of jaundice, out of which 3 neonates were full term and 9 neonates were preterm. One preterm baby had ABO incompatibility along with septicemia.
Various aggravating factors like PROM (3 cases), Toxemia of pregnancy (1 case), Prolonged labour (3 cases), Prematurity (3 cases) and birth asphyxia in 1 case was seen.
Various laboratory investigations were suggestive of septicemia with total WBC count 5000-10000/cmm. Toxic granules were seen on peripheral smear and C reactive Protein was positive in 4 cases.
Blood culture was positive in two neonates; E.Coli was isolated in both of them. Meningitis was feature in three cases with CSF picture suggestive of meningitis. All the neonates were treated with appropriate antibiotics.
Septicemia as cause of hyperbilirubinemia was found in 8% neonates by Merchant R.H. et al14,in 11.6% neonates by Verma et al15,in 5.7% neonates by Singhal et al13 and in 9.6% neonates by Narang et al12. Our ndings are in accordance with that of Marchant14, Verma15 and Narang et al12.
Rh incompatibility: Rh incompatibility was seen in eight neonates. History of affection of previous sibling was available in two cases. Direct coomb’s test was positive in all neonates. Other investigations revealed hemolytic picture on peripheral smear and high reticulocyte count. Rh incompatibility was found in 18.6% neonates by Merchant et al14, in 8.1% neonates by Singhal et al13, 2.9% by Narang et al12.In study by Verma et al159.6% neonates had Rh incompatibility. Our ndings are close to Verma et al15 and Singhal et al13.
ABO incompatibility: Incidence of ABO incompatibility was more than Rh incompatibility in our study with 18 neonates having ABO incompatibility and 8 neonates having Rh incompatibility. Direct coomb’s test was weakly positive in only 3 cases. ABO incompatibility was found in 22.6% neonates by Merchant et al14,in 22.6% neonates by Verma et al15, in 14.3% neonates by Singhal et al13.Our ndings are close to Singhal et al13.
G-6 PD deficiency: It was found in one neonate. There was history of affection of previous two male children. Baby developed jaundice between 48-72 hours. Peripheral smear was suggestive of hemolytic anemia, reticulocyte count was very high. G-6-PD de ciency was found in 2.6% neonates by Merchant et al14, in 5.1% neonates by Singhal et al13 and in 3.4% neonates by Narang et al12. Our ndings are closer to Merchant et al14.
Cephalhematoma: Cephalhematoma was causative factor in 4 neonates. Cephalhematoma as a cause of jaundice was found in 2.6% neonates by Merchant et al14, in 2.9% neonates by Singhal et al13, in 6.3% neonates by Narang et al12. Our ndings are matching with that of Singhal et al13.
Miscellaneous group: It consisted of one neonate. The baby had many congenital anomalies in the form of contractures of knee and elbow joints, craniosynostosis, ambiguous genitalia, and bilateral Grade II hydronephrosis on ultrasonography of abdomen. The mother had history of previous two intrauterine deaths. This baby died on seventh day.
Bilirubin Encephalopathy: Two babies developed bilirubin encephalopathy. Of them one was premature with ABO incompatibility and other was a term neonate with Rh isoimmunisation. The premature neonate developed signs of encephalopathy at 72 hours and term neonate after 72 hours of age. Exchange transfusion was done in both of them. The term baby also had birth asphyxia.
Verma et al51 found Kernicterus in 10.4% of cases of which maximum cases were of G-6-PD de ciency followed by idiopathic hyperbilirubinemia and Rh incompatibility.
Therapeutic Interventions: Out of the 120 neonates 16 required exchange transfusion. Maximum numbers of exchange transfusions were done in the neonates having ABO incompatibility (5) and idiopathic hyperbilirubinemia (5). The other neonates that required exchanges were of Rh incompatibility(3), Septicemia (2) and G-6-PD de ciency (1). Exchange transfusion was done when serum bilirubin level was above 20mg/dl in term babies but was done at lower serum bilirubin levels in preterm babies. Other risk factors like birth asphyxia, septicemia, hypoglycemia, and acidosis were also considered while deciding exchange transfusion.
Dikshit et al82 found the commonest condition requiring exchange transfusion was ABO incompatibility, followed by Rh incompatibility, septicemia and G-6-PD de ciency, while in study of Singhal et al1 3 common causes of hyperbilirubinemia requiring exchange transfusion were Rh incompatibility followed by ABO incompatibility and G-6-PD de ciency. Narang et al12 found that the most common cause of hyperbilirubinemia needing exchange transfusion was idiopathic (35.4%), followed by sepsis (24.1%) and G-6-PD de ciency (17.2%).
Rest of the 104 neonates in our study received either phototherapy alone or along with phenobarbitone. Phototherapy was started when serum bilirubin was found to be more than 10 mg/dl and was given for 24, 48 or 72 hrs. Though exchange transfusion was required in 5 cases of ABO incompatibility and 3 cases of Rh incompatibility, the remaining cases of ABO incompatibility (12) and Rh incompatibility (5) recovered with phototherapy alone or in some cases in combination with phenobarbitone. This indicates that phototherapy is effective in management of hemolytic as well as non-hemolytic hyperbilirubinemia of newborn.
Osborn L.M. et al92 con rmed with studies that, phototherapy is highly effective in ABO hemolytic disease of newborn.
The fall in serum bilirubin level was 2-3 mg/dl/24hrs in our study. Singhal et al52 found the fall of bilirubin level with phototherapy in idiopathic jaundice to be 2.5 1.8mg/dl, in Rh incompatibility 3.4 2.4 mg/dl, in septicemia 2.1 1.4mg/dl in ABO incompatibility 2.1 1.4 mg/dl and in G-6-PD de ciency to be 2.4 1.4 mg/dl. Our nding matches with that of Singhal et al13.
In our study addition of phenobarbitone was not associated with any signi cant additive effect as compared to phototherapy alone. This nding is similar to that Lall J.C. et al34.
Side Effects: Phototherapy: In our study, ve neonates developed loose motions and four neonates developed rash over body.
William Oh et al have found a greater stool water loss, greater insensible water loss and increased respiratory rate in phototherapy infants as compared to controls.
Exchange transfusion: In our study, one baby had cardiac arrest during exchange transfusion, 3 babies had hypoglycemia during exchange transfusion and two babies developed septicemia after exchange transfusion. However baby with cardiac arrest during the procedure was effectively resuscitated and the other complications also properly managed.
Dikshit et al in their studies found that the overall mortality in babies subjected to exchange transfusion was 10.6/100 exchange transfusions.
Lokeshwar et al in their study found incidence of procedure related complications to be 26.16% with overall procedure related morality 0.93%.
Our results are correlating with that of Singhal et al who found similar complications without any mortality.
Narang et al12 found that the most common cause of hyperbilirubinemia needing exchange transfusion was idiopathic jaundice followed by sepsis and G-6-PD de ciency. The incidence of major complication was 1.7/100 exchange transfusions.
Risk Factors:
Maternal: In the present study maximum number (11) of babies who developed jaundice had prolonged labour, 7 neonates had history suggestive of toxemia of pregnancy, 6 neonates had PROM more than 18 hrs and 4 neonates had oxytocin induction of labour.
Foetal: In 26 neonates prematurity was the aggravating factor while in 13 neonates the history was suggestive of birth asphyxia.
Narang et al12 found oxytocin induction as a cause of hyperbilirubinemia in 2.4% cases. Singhal et al13 have found prematurity as a cause of jaundice in 16.7% of neonates. They have also found birth asphyxia as aggravating factor for hyperbilirubinemia in 12.1% cases out of which maximum were in idiopathic group. Our ndings correlate with ndings observed by Singhal et al13.
Conclusion:
1.Most common cause of hyperbilirubinemia requiring exchange transfusion was ABO incompatibility and idiopathic jaundice followed by Rh incompatibility, septicemia and G-6-PD de ciency.2.Phototherapy is a cheap and effective way to reduce bilirubin levels in neonatal jaundice. It is also effective in lowering the bilirubin levels in hemolytic hyperbilirubinemia and thus reducing the need for exchange transfusion. The side effects associated with phototherapy are few and not serious.3.The addition of phenobarbitone is not having any signi cant additive effect as compared to phototherapy alone.4.Though exchange transfusion is risky procedure, mortality is nil.5.Bilirubin encephalopathy is a dreaded complication if hyperbilirubinemia is not treated in time. It is more common in premature neonates and in those with a history of birth asphyxia.
Bibliography:
1. Avery GB, Maisels MJ Jaundice , Pathophysiology and management of newborn. 5th ed. Philadelphia: Lippincott JB Company;1999.
2. Taeush,Ballard,Gleason.Avery’s Diseases of the Newborn. 8th ed. Philadelphia Elsevier;2005.
3. Anand VR, Magotra ML. Neonatal Jaundice: Its Incidence and Aetiology. Indian Pediatr Feb 1978;15(2):155-60.
4. Sharma J, Sharma R, Bahl L.Etiology of neonatal Jaundice at Shimla. Indian Pediatr Oct 1994;31:1275-78.
5. Behrmann RE,Hsia DYY. Summary of a symposium on phototherapy for hyperbilirubinemia. J Pediatr 1969;75(4):718-26.
6. Johnson L, Bhutani VK.Guidelines for the management of the jaundiced term and near term infant. Clin Perinatol Sept 1998;25(3):555-74.
7. Gathwala G,Kumar P. Neonatal Jaundice: Indian Pediatr May 1997;34:429-32.
8. Lochmann KK, Sodhi M, Singh G. Incidence of neonatal jaundice. Abstracts Pedicon 2004;158-59.
9. Ramesh Agarwal, A.K. Deorari : Unconjugated hyperbilirubinemia in newborns: Current perspective; Indian Pediatrics,39:2002;30-32.
10. Misra P. K. and Govil Y.C. : Neonatal hyperbilirubinemia; IAP Journal of Practical Pediatrics, 2 (4), 1994, 361-366.
11. Phyllis A. Denney, William D. Rhine, David K. Stevenson: Neonatal jaundice – What now ?; Clinical Pediatrics, 1995, 103-105.
12. Narang A, Gathimala G, and Praveen Kumar: Neonatal jaundice: an analysis of 551 cases; Indian Paeditrics, 2001, 68, 977-980.
13. Singhal P.K., Meherban Singh, V. K. Paul, A.K. Deorari, and M.G. Ghorpade: Spectrum of neonatal hyperbilirubinemia. An analysis of 454 cases, Indian Paediatrics, 1992, 29, 319-325.
14. Merchant R. H., Merchant S.M. and Barbar S.T.: A study of 75 cases of neonatal jaundice; Indian Paediatrics, 1975, XII(9) 889-893.
15. Verma Manorama, Jugesh Chatwal and Daljit Singh: Neonatal hyperbilirubinemia; Indian Journal of Paediatrics 1988, 55, 899-904.
Issue: July-September 2015 [Volume 4.3]
