Determinants of physical and Neurodevelopment outcome of high risk newborn with maternal and neonatal risk factors
Original Research
Abstract –
Objective: to assess developmental outcome using simpler methods like Amiel-Tison with relation to neonatal and maternal risk factors. Design: prospective study Methodology: The study was conducted at secondary care hospital in Mumbai with low resources but high patient turnover. In this study, 150 babies admitted to neonatal care unit (NCU) due to various problems were opted with consent and ethical committee clearance of the hospital. Neurological Assessment was done by Amiel-Tison method and babies screened for complications during regular scheduled follow up visits. Results: Preterm comprised 61.84% of the total cohort. Poor socioeconomic status and maternal risk factors like pregnancy induced hypertension (PIH), antepartum haemorrhage (APH) were responsible for preterm delivery. Adverse neurodevelopmental outcome in terms of developmental delay was seen in 21.66% LBW and 25.53% of preterm babies. Of total 76 samples, 18 (23.68%) had abnormal outcome.
Conclusion:
Multiple maternal risk factors and social factors increase the risk of poor neurological outcome. Simple methods like tone assessment can be used for evaluation of neurological outcome with less expertise. Early intervention helps in preventing further complications.
Key words: high risk newborn, low birth weight, prematurity, Amiel-Tison
Introduction:
Maternal, biological and social risk factors convey altered probabilities of a poor birth outcome. Poor socioeconomic status has been proved to be responsible for low birth weight (LBW) and poor developmental outcome. Early detection of developmental delay in high risk newborns group with identification of associated perinatal factors and their prevention can prevent disability in later life.1 Incidence of neurodevelopmental delay (NDD) among high-risk newborns is significantly high; with LBW, prematurity, and birth asphyxia being major contributors.2 Mortality and rehospitalisation rate is high in high risk infants, after discharge from the hospital.3 Follow-up care program for a minimum of six months after discharge from maternity hospitals may help to avoid adverse and life threatening consequences in high risk infants.4 The updated Amiel-Tison Neurological Assessment at Term (ATNA), the method used in the current study, is an extension of the French method of infant neurological evaluation initiated by Andre´ Thomas in 1949 and Saint-Anne-Dargassies in 1960.5,6 It takes five minutes to examine using the scale, thus can be implemented in clinical and research assessment.6 It is important to assess passive tone in the first year for early diagnosis of developmental disabilities and for planning early interventional therapy.7 ATNA is valuable in assessing aetiology, timing of brain lesion and follow up assessment.8 Timely and appropriate intervention can prevent or modify many of these disabilities. The neonates at increased risk of neurodevelopment disability can be identified by assessing certain perinatal risk factors and the course of their illness postnatally: a structured plan of follow-up can then be designed for them in order to assess their developmental status and identify delay at the earliest, using simplified assessment tools like Amiel-Tison. This study was carried out with objective to assess the level of NDD using simplified tool and establish an association between the risk factors and level of developmental delay.
Methods and materials:
In this prospective observational study, mortality, morbidity and developmental outcome were seen in 150 (93 male and 57 female) newborns admitted with various problems at a secondary level neonatal care unit (NCU) of peripheral hospital in Mumbai. They were followed up over a period of one and half years (18 month) of age since birth. Newborn babies fulfilling following criteria were included in the study – birth weight <2000 gm and >4000 gm with or without complications, gestational age < 37 completed weeks, Apgar Score = 5 at 5 minute, neonates with meconium aspiration syndrome (MAS) diagnosed on the basis of both clinical and radiological criteria, hyaline membrane disease, transient tachypnea of newborn (TTNB), persistent pulmonary hypertension of newborn, both early onset and late onset sepsis, hyperbilirubinemia requiring phototherapy and neonatal seizures due to any cause. Exclusion criteria were term normal baby weighing between 2000 to 4000 gm, deaths within hospital, multiple congenital malformation and babies who were transferred to tertiary care centre for intensive and ventilator support. Regular follow up visits were planned for all the discharged babies at the age of six weeks and three, six, nine, twelve, eighteen months. Detailed birth history, maternal risk factors, mode of delivery, resuscitation and socioeconomic factors were also taken into account. During each follow up visit, anthropometry, neurological assessment, achievement of milestones with respect to corrected gestational age, vision and hearing assessment were done. Special emphasis was given to detailed tone assessment by Amiel Tison method. Ultrasonography of cranium at 6 week, sequential examination for retinopathy of prematurity (ROP), hearing assessment with Brain stem evoked response audiometry (BERA) and management of minor illness were done during the follow up. A standard examination protocol was used during visitation schedule in the form of ATNA. Data was collected by minimum 1 year follow up of infants and percentage of mortality, morbidity, neurological disability, developmental quotient (DQ) and rehospitalisation rate noted.
Observation and results: Out of total 150 samples, 71 infants didn’t follow the predefined follow up schedule and three expired from the total cohort before the third follow up. Total dropout at scheduled third and fifth follow up was 44.66% and 47.33% respectively. Further study was restricted to 76 infants (50.66%) who followed up regularly till one year of age and out of them only 14 babies completed follow up till 18 month of age. Dropout was high among females (52.63%) compared to males (44.83%).
Out of the total followed up cohort of 76 babies, 50 (65.78%) were male and 29 (38.15%) were female. Among maternal risk factors Anaemia 13 (16.45%) and pregnancy induced hypertension (PIH) 6 (7.59%) were more frequent (table: 1).
When maternal risk factors were compared with outcome of babies then out of 13 mothers who had anaemia; 11 (84.61%) babies were LBW and 07 (53.84%) were preterm. And all the babies born to mother with PROM, APH, multiple gestation, tuberculosis, HIV infection, syphilis were LBW and preterm. Almost 93.67% mothers were from low socioeconomic group which had adverse effect on pregnancy outcome as 47 (61.84%) babies were preterm and 60 (78.94%) babies were LBW.
Among neonatal risk factors Prematurity 47 (61.84%) and LBW 60 (78.94%) were frequently observed followed by hyperbilirubinemia, sepsis, respiratory distress and neonatal seizure. (table: 2)
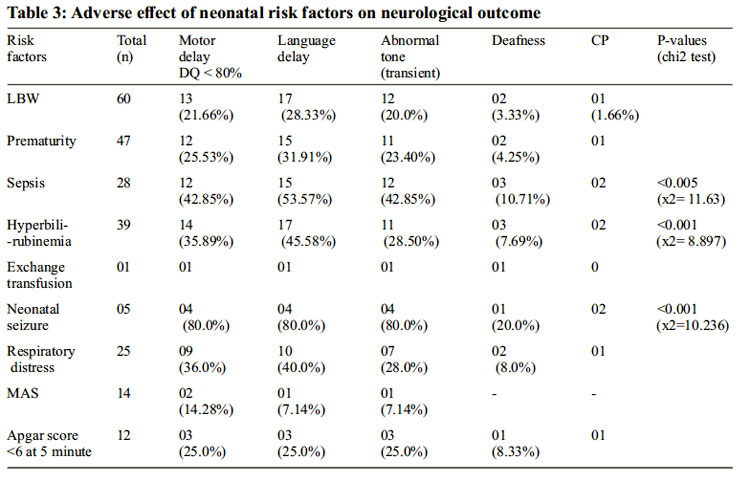
Out of total 60 LBW, 13 (21.66%) had delayed motor mile stones, 17 (28.33%) had language delay, 12 (20.0%) had transient abnormalities of tone during early infancy, 2 (3.33%) had deafness and one developed cerebral palsy (CP). When 47 preterm were observed regarding their abnormal neurodevelopmental outcome; delay in motor and language milestones was noted in 12 (25.53%) and 15 (31.91%) of them, respectively as shown in table-3.
Transient tone abnormalities were seen in 12 (15.17%) which was noticed between ages of 3-6 months. Out of these 12 infants, all were LBW, 11(91.66%) were premature and 2 of these had low Apgar score at birth. By the end of one year, no obvious abnormality was detected. DQ <80 was present in 15 (19.73%) cases and 17 (22.36%) had language delay. None of the babies had developed Retinopathy of prematurity.
Mean length velocity in small for gestation age (SGA), appropriate for gestation age (AGA) and large for gestation age (LGA) at one year of age were 22.9, 24.2 and 23.2 cm/year respectively. When seen in National Center for Health Statistics (NCHS) growth charts, (15 out of 25) 60% SGA babies and (16 out of 45) 35.5% AGA babies had length below third centile at one year of age. Similarly, 2 (8.0%) SGA babies and 7 (15.5%) AGA babies achieved length between 50 and 97 centiles at their first birthday. Catch up growth was not good among LBW and VLBW babies as (37 out of 60) 61.66% LBW babies and (16 out of 17) 94.11% VLBW babies had weight below third centile at one year of age.
Relation of neonatal morbidities with DQ is shown in table no 4. Statistical significant correlation of neonatal risk factor and DQ was found between sepsis, seizurs and hyperbilirubinemia with significant p-values of <0.005 (x2 = 11.63), <0.001 (x2 = 10.236) and <0.001 (x2 = 8.897) respectively. Out 76 babies, 18 (23.68%) had abnormal outcome in form of DQ < 60.
Discussion:
There are few studies to tell correlation between neonatal outcome with neonatal and maternal risk factors in low resource secondary level NCU. This study had attrition rate of 50.66% at the end of one year. Poverty, illiteracy, social customs, poor transport facilities, lack of awareness amongst parents, migration of families who were working at construction sites were reasons for poor follow up. According to a study of Australia, high-risk children have long-term medical, developmental and psychological adverse outcomes that consume extensive health and education services as they grow older which can be prevented by structured follow up scheme and early intervention.9 Drop out 33% during follow up was also seen in another retrospective study conducted in NICU, Government General Hospital, Kakinada over a period of 18 months from March 2012 to August 2013.10 In the present study the main reasons for lost to follow up were mothers who came for delivery at their mother’s home went back to their husband’s home, parents of infant working on daily wages and have to move one another places for earnings. In another study of developing country, lost to follow up rate was 26% due to divorce, loss of employment or death of parents.11
Out of total 76 enrolled, 46 (76.66%) LBW were male and 14 (23.33%) LBW were female. In our study, LBW (78.94%) and VLBW (21.05%) formed the largest group of the subject. Preterm comprised 61.84% of the total cohort. Male LBW had poorer neurological outcome than female as consistent with Janet L et al and Nandita C et al.12,19 Apart from poor socioeconomic status, maternal risk factors like PIH, APH were major risk factors for preterm delivery which was similar to many other studies.13 This is supported by a study done in South India where most common risk factors associated with preterm birth were PIH (21.4%), height <1.50 meter (16.8%), PROM (17.5%), and fetal distress (14.9%).14 Nandini Naskar et al in study of 744 LBW babies reported relation of poor socioeconomic status in 40.86% cases.15 But in a study of Luckhnow, 22% deliveries were preterm; PROM and maternal infection were attributed for the cause of the same.16 In another South African study of 76 VLBW, in which follow up rate was 66% and out of which 17% had developmental delays/ disabilities.17 In a study done in 1654 newborns from Bangladesh with poor socioeconomic status, 46.4% were LBW (< 2500 g) and 69.6% of the newborns were SGA.18
Adverse neurodevelopmental outcome in terms of developmental delay was seen in 21.66% LBW and 25.53% of preterm babies which is supported by study of Nandita Chattopadhyay et al. 19 In contrast, a prevalence rate of developmental delay was between 5.7 and 7.0 % in Norwegian preterm infants between 4 and 12 months of age.20 Spastic diplegic CP, intellectual disability, ROP and hearing impairments are the main neurodevelopmental disorders associated with prematurity.21
In a cross sectional study of west India, conducted with 200 babies neonatal risk factors like preterm, IUGR, respiratory distress, sepsis, seizures in neonatal period showed significant p value for developmental delay.22
On reviewing the data of 15 years, Arend F Bos found the prevalence of fine motor skill impairments in very preterm infants lied between 40% and 60%.23 In this study, two infants had meningitis out of which one developed severe motor retardation and other developed spastic diplegia. It is supported by Tatina B et al according to which neonatal meningitis leads to deafness, blindness, cerebral palsy, seizures, hydrocephalus or cognitive impairment in approximately 25–50 % of survivors.24
Thirty-nine of total cohort developed treatable hyperbilirubinemia out of which, 14 (35.89%) had poor neurodevelopmental outcome with significant p-value and 3 (7.69%) developed sensory neural deafness. Paul V. K. Et al, in their study found adverse outcome in 13.5% of infants with hyperbilirubinemia.25 According to US study done at 12 centres from 1959 to 1974 in 41,324 samples, no correlation was found between neonatal hyperbilirubinemia and neurodevelopmental outcome which was checked with respect to Intelligence Quotient (IQ) assessment at 7 years age and sensorineural hearing loss at age 8 years.26 In the present study, 25 babies with respiratory distress, 36% had adverse neurodevelopmental outcome. It was high value as compare to other studies.25 In this study, 12 babies had birth asphyxia from which two developed HIE II and 3 (25%) had poor neuodevelopmental outcome which is supported by another study of western India, in which out of total 45 babies with severe birth asphyxia, 13 (28.8%) developed HIE grade II and III separately.27
Among infants with seizures, 80% had abnormal outcome with significant p- value. Two of the seven infants with neonatal seizures expired during second month of life. Infants with neonatal hypocalcemic seizures had normal outcome.
In present study, there were 2 cases of frank Cerebral Palsy with overall incidence of 2.63%, which is consistent with both national and international studies. In India incidence of CP remain three per thousand live births in last two decades.28 In this study, 12 babies had transient tone abnormalities, 15 had motor dysfunction and 17 had delayed language milestone but none of these showed sign of frank CP; hence labelled to have minor neuromotor dysfunction. Such transient abnormalities are described by Amiel Tison and by Chaudhary et al where Amiel Tison method of neurological assessment was compared with Bayley scale of infant development.7, 29, 30 Varsha Amin et al in 2004 found Amiel Tison scale more specific than Bayley scale of infant development (BSID). Features described by Amiel Tison are easy to use thus can be used by untrained hands.31 Thejus T. Jayakrishnan et al compared visual and the goniometric assessment of adductor and popliteal angles which is important component of Amiel-Tison method and found a significant difference between the two methods. Thus by these two methods angle difference between the joints were significant.32 Amiel-Tison scale can be used by occupational therapists in infant assessment and intervention because of its easiness.33 The worst outcome was found in infants who had more than three comorbid condition during NICU stay and whose NICU stay was prolonged for more than 7 days. Most of the SGA babies remain below third percentile of length (NCHS standard) at the end of first year compared to normal population may be because of the poor catch up growth due to poor income resources. At the end of this study, 58 babies (76.31%) were free of any neurodevelopmental deficit.
Conclusion
Multiple risk factors increase the risk of poor developmental outcome. Social variables like poor socioeconomic status and illiteracy are significantly associated with adverse neurodevlopmental outcome but longer follow up are required to establish the aspect. Maternal risk factors though did not have direct effect on neurodevelopment outcome but it contributed increase in incidence of prematurity and LBW. Neonatal sepsis, hyperbilirubinemia and neonatal seizures had shown statistically significant correlation to poor neurodevelop-mental outcome. Poor physical growth is observed in SGA babies as compare to AGA babies. Amiel Tison scale can be used till one year of age for easier assessment of developmental outcome even by less trained hands at low resource setups.
Early intervention prevents the poor outcome with regard to neurological assessment. Invasive intervention and prolonged hospital stay had significant effect on morbidity. Prematurity per se is a relatively weak risk factor, rather the neonatal complications of prematurity have more predictive value for developmental outcome than the prematurity alone. Most NDDs go undetected in the early years of life. Improved perinatal care, early detection, and early intervention at the grassroot level will bring down incidence of developmental challenges in this vulnerable group.

References :
1. Nandita Chattopadhyay, Kaninika Mitra. Neurodevelopmental outcome of high risk newborns discharged from special care baby units in a rural district in India. Journal of Public Health Research 2015; 4:318,7-12
2. Modi R, Patel J, Mishra A. Neurodevelopmental outcome of high-risk newborns discharged from NICU in a tertiary-care hospital of western India. Int J Med Sci Public Health 2016;5:1350-1354
3. Sudha Chaudhari, Sujata Kulkarni, Anand Pandit et al. Mortality and morbidity in High Risk Infants during a six year follow-up. Indian Pediatrics 2000;37: 1314-1320
4. Mohammad Heidarzadeh, Behzad Jodeiry, Mohammad Baqer Hosseini, et al., “High Risk Infants Follow-Up: A Case Study in Iran,” International Journal of Pediatrics, vol. 2015, Article ID 817540, 5 pages, 2015. doi:10.1155 /2015/817540
5. Amiel-Tison C. 2002a. Update of the Amiel- Tison Neurologic Assessment for the Term Neonate or at 40 Weeks Corrected Age. Pediatr Neurol 27:196 –212.
6. Julie Gosselin, Sheila Gahagan, and Claudine Amiel-Tison. The Amiel-Tison neurological assessment at term: conceptual and methodological continuity in the course of follow-up. Mental retardation and developmental disabilities research reviews 11: 34 –51 (2005).
7. Sudha Chaudhari and Bhushan Deo. Neurodevelopmental Assessment in the First Year with Emphasis on Evolution of Tone. Indian Pediatrics,(43),2006,527-534.
8. Paro-Panjan, D., Neubauer, D., Kodrie, J. and Bratanic, B. (2005), Amiel-Tison Neurological Assessment at term age: clinical application, correlation with other methods, and outcome at 12 to 15 months. Developmental Medicine & Child Neurology, 47: 19–26. doi:10.1111/j.1469-8749.2005. tb01035.x.
9. Lex W Doyle, Peter J Anderson, Malcolm Battin et al. Long term follow up of high risk children: who, why and how? Doyle et al. BMC Pediatrics 2014, 14:279 .
10. Kakinada D. Manikyamba, N. Madhavi, A. Krishna Prasad, I.V. Padmavathi, Anitha. Morbidity and Mortality Profile of LBW Babies and Their Growth and Neurodevelopment Outcome at 1 year- NICU, Government General Hospital Kakinada. Sch. J. App. Med. Sci., July 2015; 3(4B):1721-1725.
11. R. A. Kambarami, O. Chidede, N. Pereira. Long-term outcome of preterm infants discharged home on kangaroo care in a developing country. Annals of Tropical Paediatrics (2003) 23, 55–59.Janet L. Peacock
12. , Louise Marston, Neil Marlow et al. Neonatal and infant outcome in boys and girls born very prematurely. Pediatric Research (2012) 71, 305–310
13. Devi Meenakshi K, Arasar Seeralar AT, Padmanaban S. Clinical profile and factors determining outcome of intramural very low birth weight babies in a tertiary care centre: a retrospective study. Int J Res Med Sci 2017;5:520-4. Chythra R. Rao
14. Lara E. E. de Ruiter, Parvati Bhat et al. A Case- Control Study on Risk Factors for Preterm Deliveries in a Secondary Care Hospital, Southern India. ISRN Obstetrics and Gynecology Volume 2014, Article ID 935982, 5 pages http://dx.doi.org/10. 1155 /2014/ 935982.
15. Naskar N, Swain A, Das KD, Patnayak AB (2014) Maternal Risk Factors, Complications and Outcome of Very Low Birth Weight Babies: Prospective Cohort Study from a Tertiary Care Centre in Odisha. J Neonatal Biol 3:142. doi:10.4172/2167-0897.1000142.
16. Singh Uma, Singh Nisha, Seth Shikha. A prospective analysis of etiology and outcome of preterm labor. J Obstet Gynecol India Vol. 57, No. 1: January/February 2007 Pg 48-52.
17. Adu-Boahene, Akua, “Outcome of Extremely Low Birth Weight Infants In A Resource Limited Setting” (2011). Yale Medicine Thesis Digital Library. Paper 1534.
18. Shams E Arifeen, Robert E Black, Laura E Caulfield et al. Infant growth patterns in the slums of Dhaka in relation to birth weight, intrauterine growth retardation, and prematurity. The American Journal of Clinical Nutrition 2000;72:1010–7.
19. Chattopadhyay N, Mitra K. Neurodevelopmental Outcome of High Risk Newborns Discharged from Special Care Baby Units in a Rural District in India. Journal of Public Health Research. 2015;4(1):318. doi:10.4081/ jphr.2015.318
20. Lisbeth Valla, Tore Wentzel-Larsen, Dag Hofoss, and Kari Slinning. Prevalence of suspected developmental delays in early infancy: results from a regional populationbased longitudinal study.
21. Farin Soleimani, Farzaneh Zaheri, Fatemeh Abdi. Long-Term Neurodevelopmental Outcomes after Preterm Birth. Iran Red Crescent Med J. 2014 Jun; 16(6): e17965.
22. Hetal Vora, Priti Shah, SH Mansuri. A study on developmental delay among children less than 2 year attending well baby clinic – prevalence and antecedents factors. International Journal of Medical Science and Public Health. 2013, Vol 2, Issue 4; 1084-1087.
23. Arend F Bos, Koenraad N J A Van Braeckel, Marrit M Hitzert et al. Development of fine motor skills in preterm infants. 2013 Mac Keith Press, 55 (Suppl. 4): 1–4
24. Tatiana Barichello, Glauco D. Fagundes, Jaqueline S. Generoso et al. Pathophysiology of neonatal acute bacterial meningitis. Journal of Medical Microbiology (2013), 62, 1781– 1789.
25. Paul V K, Radhika S, Deorari A K, et al. Neurodevelopmental outcome of ‘at risk’ nursery graduates. Indian Journal of Pediatrics 65(6): 857-862.
26. Newman TB, Klebanoff MA. Neonatal hyperbilirubinemia and long-term outcome: another look at the Collaborative Perinatal Project. Pediatrics. 1993 Nov;92(5):651-7.
27. Pareshkumar A. Thakkar, Paresh Valia, Niyati Parmar et al. Clinical profile, outcome and clinical indicators for poor prognosis in full term babies born with severe birth asphyxia: study from tertiary care hospital from western India. International Journal of Contemporary Pediatrics. 2017 Mar;4(2):470-476.
28. Umesh Isalkar. Incidence of cerebral palsy remains unchanged in India. The Times Of India Pune;Date: Oct 4, 2010;Section: Times City;Page: 4.
29. Amiel Tison C, Grenier: Neurological assessment within the first five year of life, early assessment and outcome. Dev. Med. Ch Neuro 1986 28: 671-82
30. Chaudhari S, Shinde S V, Barve S S et al. Longitudinal follow up of neurodevelopment of high risk neoborns: A comparison of Amiel- Tison’s method with Bayley’s scale of infant development. Indian Pediatrics, 1990, vol 27, Aug 1990.
31. Mohit Mittal, Bhavana Lakhkar. Physical features and neurodevelopment outcome in high risk newborn. Pediatric Oncall Journal. September 1, 2011, Vol 8, Issue 9, Art 60.
32. Jayakrishnan TT, Sharma S, Gulati S, Pandey RM, Wadhwa S, Paul VK. Agreement between visual and goniometric assessments of adductor and popliteal angles in infants. Journal of Pediatric Neurosciences. 2013; 8(2):93-96. doi:10.4103/1817-1745. 117834.
33. McCarraher-Wetzel AP, Wetzel RC.A review of the Amiel-Tison neurologic evaluation of the newborn and infant. Am J Occup Ther. 1984 Sep; 38(9):585-93.



Issue: July-September 2017 [Volume 6.3]
