Targetting Early Neonatal Mortality Key to Reduce Infant Mortality Rate In India (Beyond Mayurbhanj Model)
Original Research
Abstract:
The National IMR ( Infant Mortality rate) is regressing but ENMR (Early Neonatal Mortality rate) is not showing reduction in the same way as Late Neonatal Mortality or Post Neonatal Mortality. The crux of the Problem is mostly around Birth Asphyxia, Neonatal Infection (Sepsis) and prematurity. With adequate perinatal services most of them could have been prevented. Stress is laid upon birth asphyxia; because it causes death or disability in survivors. Sepsis treated early or if prevented produce good dividend and the survivors are not very much handicapped. Improved perinatal services like ante-natal care for the mothers and introduction of Neonatal resuscitation supposed to have reduced ENMR. However it does not look like effective, may be due to lack of appropriate application. Full term normal birth weight neonates dying of Birth Asphyxia could be prevented with assisted delivery in time. Sepsis can be prevented with properly chosen prophylactic antibiotic therapy. Prematurity without the above two adversities is bound to result in less neonatal loss, seen over the years. In low birth weight babies with or without prematurity, the probable cause might be placental insufficiency due to various maternal causes, these can be tackled with proper follow up and better obstetric care protocol. As the deliveries now are mostly institutionalized and ASHAs give adequate follow up to the expectant mothers it will be easy to tackle the issue of complicated delivery with timely referral to the nearby properly staffed hospitals. As a conservative estimate, with alteration of the present system and support, the neonatal mortality rate could be reduced by 11, from the present 41 to 30 straight away.
Key Words : Early neonatal mortality rate, Late Neonatal mortality rate,infant mortality rate , HIE (Birth Asphyxia), Sepsis, Prematurity.
Introduction:
India has witnessed dramatic reduction in under five mortality and IMR in past two decades. Neonatal mortality has reduced much less than Post-neonatal deaths. In 1990, 41% of under five deaths are due to neonatal mortality which has increased to 56% by 2012. Still births are largely invisible(1) by 2015 the under five mortality was 47.70, IMR 37.90 and Neonatal mortality 27.70. 73% of IMR is due to neonatal loss. This area needs intensive attention.(2) From 1990 upto 2000, the reduction in neonatal mortality was rather slow; from 2 to 3%. After 2000 with inputs from both Government and Private Sector, the Neonatal Mortality is decreasing at more than 3% every year. The late neonatal mortality has shown a reduction of 50% between 2000 and 2012. But the early neonatal mortality except for the year 2000 to 2001, has not shown any substantial decline. (3)
The average annual reduction in late NMR and Post NMR are 5.8% and 5.1% respectively while the average annual reduction of early NMR is 2.8% from 2000 to 2012(3). About three fourth (72.9Z%) neonatal deaths occur in the 1st week of life. 2nd week accounts for 13.5% and last 2 weeks account for 13.5% mortality. 50% of the early neonatal deaths occur in the first 24 hours of birth. Broadly four categories of diseases are responsible for early and late neonatal deaths; they are birth asphyxia, prematurity, sepsis and malformations. Baqui AH et al(4) provided data on timing of cause specific neonatal deaths in rural India.
Almost all deaths consequent upon birth asphyxia (97.8%) occur within the 1st week of life 70% of these occur within 1st 24 hours. About three fourth of the prematurity deaths (74.8%) occurs in the 1st week 30% occurring within 1st 24 hours. Less than 50% of neonatal deaths due to Sepsis occur in 1st week and 30% in 2nd week. Three fourth of the deaths due to Malformation occur in the 1st week with nearly half being contributed within 24 hours (5).
From the above it is clear that early neonatal mortality and more so, within 1st 24 hours is of concern and a key to reduce the IMR. Much of these deaths are the result of prolongation of adverse perinatal events. Introduction of National Health Mission with ASHA workers, better health awareness, better curative services and improved access to services from Health system have ofcourse paid dividends.(6) Therefore it will not be difficult to count every delivery and introduce plan of action to reduce 1st week morbidity and mortality.
Neonatal mortality is influenced by various socio economic and demographic factors. Neonatal mortality in urban area is far less than the rural area. Though the number is less, yet the causes are similar. Report by from Mumbai Slum(7) revealed 28 percent intrapartum related deaths, 23 percent prematurity and 22 percent infection related neonatal deaths. Death from birth asphyxia was reported to be 39% from Vellore with 21% from Prematurity. (8)
Aims and Objectives:
Therefore it was decided to analyze neonatal deaths from 5 referral centers across India. Focus was given on birth asphyxia (HIE), sepsis and prematurity; where death could have been prevented by early intervention. In a predesigned format, retrospective study was undertaken at :
1. Hi-tech Medical College, Bhubaneswar, Odisha.
2. Burdwan Medical College, Burdwan, West Bengal.
3. MGM Medical College, Navi-mumbai, Maharastra.
4. Nalanda Medical College, Patna, Bihar.
5. Patna Medical College, Patna, Bihar.
During analysis all cases having birth asphyxia the cause was tabulated under asphyxia even though other two causes might be oprating. sepsis was calculated excluding those tabulated under birth asphyxia. Premature babies without asphyxia or sepsis were counted as prematurity. This will give an insight to the preventable causes and early neonatal death.
The above three causes account for 78% neonatal deaths in India (9)
Observations:
A total of 4361 cases of birth asphyxia were analyzed. There were 2311 (53%) male and 2050 (47%) female. 1903 (43.64%) cases were below 2.5 kg and 2458 (56.36%) were above 2.5kg body weight. 2401 (55.01%) neonates were full term and 1960 (44.95%) were below 37 weeks of Gestation (Preterm). There were 1261 (28.92%) deaths due to birth asphyxia. Out of the 1261(28.92%) who died, 718 (56.94) were male and 543 (43.06%) were femail. 740 (58.69%) neonates with birth weight more than 2.5 kg died where as 521 (41.31%) below 2.5 kg died. 833 (66.06%) neonates having more than 37 weeks gestational age died as compared to 428 (33.94%) prematures.
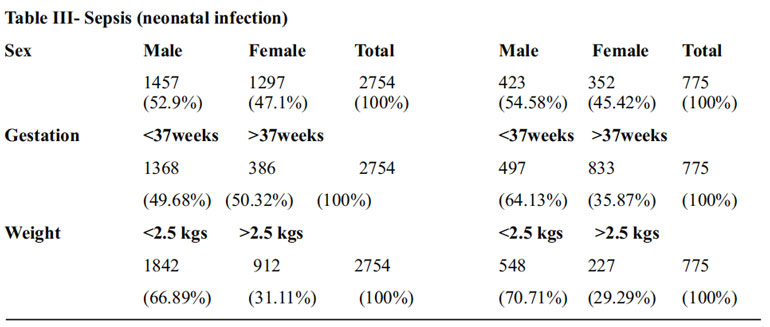
A total of 2754 cases of neonatal sepsis were studied. There were 52.9% males, 47.1% were females. 1386 (50.32%) full term neonates and 1368 (49.68%) were prematures having sepsis. 912 (31.11 %) neonates with birth weight more than 2.5 kg and 1842 (66.89 %) neonates with birth weight less than 2.5kg had Sepsis. A total of 775 (28.14%) cases died of Sepsis. 497 (64.13%) cases were Preterm babies and 278 (35.87%) were term. Out of the total deaths from Sepsis, 548 (70.71%) were below 2.5 kg of birth weight and 227 (29.29%) were more than 2.5 kg birth weight.
Prematurity– A total number of 4145 (94.84%) cases were due to prematurity without having birth asphyxia or sepsis admitted during the period neonates weighed less than 2.5 kg and 214(5.17%) weighed more than 2.5kg. Total number of death due to Prematurity was 470 (11.34%). 21 (4.47%) neonates having more than 2.5 kg weight died where as 449 (95.53%) having birth weight less than 2.5 kg expired. In one institution 39.6% neonates with birth weight 1.5 to 2.5 kg expired, the salvage rate being upto 60% and below 1.5 kg the salvage rate is roughly 40%.
Selection of Cases:
The cases are selected according ability to salvage and prevention potential. Irrespective of gestational age, Weight and presence of Sepsis, birth Asphyxia is computed as the lone cause as it is to a large extent preventable. Even treatment may salvage them but with poor life quality. Sepsis is taken as diagnosis without birth Asphyxia in spite of associated prematurity, which can be prevented to some extent and treated to a large extent. Prematurity is computed for all the new born admitted below 37 weeks of gestation without Asphyxia and Sepsis.



Discussion: Analysis of neonatal mortality in India reported by Liu et al (10) in 2012 with analysis from 2000 to 2010 showed preterm 35% Infection 33%, Birth Asphyxia 20%, Malformation and other causes 12%. Over the years the proportion of three major causes are changing as in this series 50.32% death due to birth Asphyxia tops the list . Infection with 30.93% has not changed significantly but prematurity without the above two major complications had shown a dramatic reduction to 18.76%. This warrants a change in the programme and attitude towards preventing neonatal deaths.
The early neonatal mortality rate from 2001 to 2008 is almost static with marginal reduction of one per thousand over the following years. From 27 per 1000 in 2001 it got reduce to 23 per 1000 in 2012 where as the late NMR has decreased by 50%. The death rate from 1 month to 1 year also has a reduction of 50% from 2000 to 2012.(3) This does mean that the efforts and programmes launched to reduce early neonatal mortality are ineffective or partially effective. The two most important initiatives are encouragement of Institutional delivery and Neonatal resuscitation programmes. Both are reportedly successful but the result for which the programmes were initiated has not shown appreciable effect, on early newborn survival.
The reported mortalities from 5 hospitals indicate that birth Asphyxia is the major concern at present. The crux of this problem lies in the perinatal period. Those who die from HIE, 66.06% are term babies with 58.69% having normal birth weight. With adequate care around birth these deaths could have been prevented. Early planning for assisted delivery and at birth neonatal resuscitation with trained hands could help in minimizing the loss. A cent percent effective programme could reduce IMR by 6.9 most of which would be in early neonatal period. Rest 34 to 41% might be due to intranatal Asphyxia mostly due to placental cause. Few could have been salvaged with control of pregnancy induced hypertension, eclampsia/pre-eclampsia and improvement of nutrition.
Neonatal Sepsis is the 2nd highest cause of newborn fatality. Administration of oral cotrimoxazole and injectable gentamycin in suspected cases had reduced neonatal mortality by 62.2% (11). In this series 30% are term babies with adequate weight. With early intervention they could have been saved. Many from the premature and low birth weight who are not in the extreme end could have been salvaged. This area has the potential of preventing 60% deaths due to infection which ultimately will reduce IMR by 4.14. Parameters for early diagnosis of Sepsis or Suspected Sepsis should be worked out and antibiotics should be administered as per protocol. Probably Gentamycin ones a day with adequate dose for 5 days will serve the purpose. As every child is getting Vit K injection, it will not be difficult to give the antibiotics by field staffs. The morbidity and mortality from Vit K deficiency (Haemorrhagic disease of the newborn) needs elaboration. In early HDN the mortality is negligible and is very much treatable. The Late onset HDN has an incidence of 4.4-7.2/100,000 births in children without Vit K injection at birth. With Vit K injection it got reduced to 1.4-6.4/100,000 births.(12) It is evident that half of these babies get intracranial haemorrhagic (13) it is expected that maximum of 3.5/100,000 will get intra cranial haemorrhage. The mortality for ICH being 33%, 1.55/100,000 are expected to die it Vit K is not administered. With Vit K administration the incidence has decreased to 1.4-6.4/100,000. Taking the average to the lower side i.e. ICH is expected in 1.5/100,000 births and mortality is expected to be 0.5/1lacs.thus with administration of 1 injection of Vit. K at birth the salvage rate is 1/100,000.Again Vit K deficiency bleeding can be prevented by administration of Vit. K to the mothers during last 2-4 weeks of Pregnancy.(14) In Sepsis the expected salvage rate is of 4.14 of IMR. For 1 Lac births the number where death can be prevented will be 414. Therefore selectively giving 5 injections at birth will yield dividend of 414 times.
The proportion of death from prematurity is declining. The change is perceivable with 18.76% in this series. It denotes our post natal management is efficient. Further input can be given to reduce it further without compromising the quality of life.
Conclusions: This multicentric study shows
1. The neonatal mortality can be reduced to by 11/1000 with strategic changes in our ongoing programmes.
2. Most of the reduction will be in early neonatal mortality which is not significantly affected till date.
3. Parameters for assisted delivery have to be defined and tested in the field.
4. Prophylactic antibiotics to neonates with suspected Sepsis is to be formulated. Field trials with paramedical upto ASHA workers deemed to be necessary.
5. Prospective field investigations are necessary to confirm these findings.
What this study adds:
1. Birth Asphyxia stands as the major killer in first week (Early neonatal Period) and contributes for highest number in neonatal deaths.
2. There is appreciable reduction in mortality due to prematurity.
Contribution of authors-All authors worked in their institute
Funding – None
Competing and conflict of Interest – None
References:
1. Indian Newborn Action Plan. Ministry of Health and Family welfare, Government of India, Sept, 2014. Situational analysis Page 24-30.
2. Demography of India. Wikipedia.http//enwikipediaorg.
3. SRS Statistical reports (2000-2012)
4. Baqui AH, Darmstadt GL, Williams EK et al. Rates, timing and causes of Neonatal deaths in rural India: implications for neonatal health programmes. Bull world Health Organ. 2006;84: Page 706-713.
5. State of India’s Newborns 2014.
6. Evaluation study of National Rural Health Mission (NRHM) in seven states, Planning Commission, Government of India; 2011, February.
7. Bapat U, Alcock G, More N et al. Still births and newborn deaths in slum settlements in Mumbai, India: A Prospective verbal autopsy study. BMC Pregnancy child birth 2012; 12 page 39.
8. Vaid A, Mammen A. Infant mortality in an urban slum. Ind J Pediatric 2007; 74 Page 449- 454.
9. Causes of Neonatal and child mortality in India: A Nationally representative mortality survey. The million death study collaborators. The Lancet 27 No 3, 2010, Vol 37 (97755) : Page 1853-1860.
10. Liu L, Johnson HL, Cousens S et al – Global, regional and National causes of child mortality: An updated systemic analysis for 2010 with time trend since 2000. Lancet 2012; 397: Page 2151-2161.
11. Bang AT, Bang RA, Reddy M et al. Reduced incidence of neonatal morbidities: effect of home based care in rural God Chiroli, India. Journal of Perinatology 2005 ; 25 Page 551- 561.
12. Takahasi D, shirahata A, Itoh S etal. Vit K prophylaxis and Late vit K deficiency bleeding ininfants: Fifth nation wide survey in Japan. Petriatr Int. 2011 Dec. 53(6): 897-901.
13. Pichlor E, Pichlor L. The Neonatal co regulation system and vit K deficiency bleeding – a mini eveiw. Wein Med. Wochenschr. 2008. 158(13-14):385-395.
14. Nimavat JD. Haemorrhagic disease of Newborn. Emedicine. Medscape.com /article/974489-overview updated Jan. 02,2016.
Issue: January-March 2017 [Volume 6.1]
