Clinical profile of Pediatric HIV-TB Co-infection in Post-ART Era – A Prospective Cohort Study
Original Research
Abstract
Background: Tuberculosis in India is an uncontrolled epidemic across all sections of society, despite efforts from government of India, World Health Organisation and various state bodies and our country share largest number of multidrug resistant tuberculosis. Little is known about clinical presentation and outcome of HIV/TB co-infection in children on anti-retroviral therapy. TB detection centre across the country laid emphasis on smear positivity but in HIV infected children, extrapulmonary TB is more common than Pulmonary TB. Moreover, sputum expectoration is not possible satisfactorily below 8 years of age.
Aims and objective: Clinical profile of various types of Tuberculosis seen in a cohort of HIV infected children on anti retroviral therapy (ART) prospectively over a span of mean follow up period of eight years.
Method: Seventy eight HIV positive children below 18 years, on regular follow up at a private HIV clinic of Eastern Kolkata and HIV clinic of Institute of Child Health, Kolkata from the year 2008 to 2016. All children were on ART in a phased manner from apex referral centre, Medical college, Kolkata which was renamed as center of excellence ( COE) for Pediatric HIV by Ministry of Health, Government of India. Complete ART enrollment was done and they are on day to day follow up.
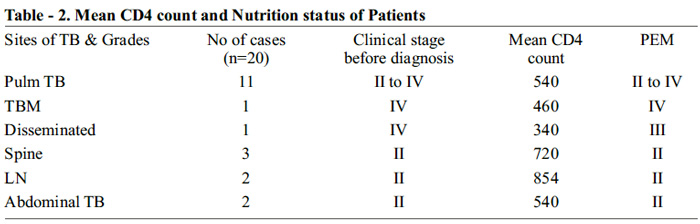
Result: Out of seventy eight HIV affected children on ART twenty were diagnose as HIV-TB co-infection on prospective follow up. Data were analysed with respect to diagnosis, clinical feature, immunological status, course and treatment of tuberculosis. Highest numbers of TB cases in this cohort of pediatric HIV on HAART were Pulmonary TB 11 (55%) followed by TB spine 3(15%). Abdominal and Lymph node TB cases show equal number of 2 (10%) each. However Tubercular meningitis (TBM) and disseminated TB contribute to 1 (5%) case each. CD4 count has no direct co-relation with the anatomical sites of Tubercular disease. 55% of cases were Pulmonary TB where mean CD4 observed were 540, similarly TB spine, Abdominal and Lymphadenitis, mean CD4 recorded was 704. Whereas only 10% of cases with TBM and Disseminated TB had mean CD4 count below 500.
Conclusion: We report high incidence of TB in HIV infected children. The diagnosis remains as a challenge where both diseases share overlapping signs and symptoms. Contrary to earlier belief, despite high CD4 count or immunological recovery occurrence of TB is still very high.
Key words: ART: Anti retroviral therapy, HIV: Human Immunodeficiancy virus, TB: Tuberculosis.
Introduction:
India has one of the largest number of tuberculosis cases globally1,2. According to WHO TB fact sheet 2015, one in three HIV death is due to Tuberculosis. HIV TB co-infection is a two way sword, where presence of one increases pathogenicity of the other. As pre global Tuberculosis report of WHO 2013, three million cases of Tuberculosis are missed or lost in the follow up.3 This contribute to emergence of multidrug resistant mutant. Geographically, the burden of TB is highest in Asia and Africa. India and China together account for almost 40% of the world’s TB cases. Worldwide, 3.7% of new cases and 20% of previously treated cases were estimated to have MDR-TB. Drug-resistant TB (DR-TB) threatens global TB control and is a major public health concern in several countries. As per latest search for drug resistant TB by RNTCP 2015 in four metro cities of Kolkata, Hyderabad, Chennai and Delhi, 9% of pediatric tuberculosis cases are resistant to rifampicin. Due to nonspecific symptoms, tuberculosis is often missed in children. The presence of Tuberculosis in HIV infected children increases both morbidity and mortality to a greater extent. Pediatric tuberculosis and HIV shares common and overlapping signs and symptoms which leads to delayed diagnosis4 or missed cases. TB detection centres across the country laid emphasis on smear positivity but in HIV infected children, extra-pulmonary TB is more common than Pulmonary TB. Moreover, sputum expectoration is not possible below 8 years of age. There are very limited descriptive study, which elaborates clinico-immunological picture of Tuberculosis in HIV infected children. The present study attempted to elaborate the spectrum of HIV with TB co-infection.
Aims and objectives: Clinical profile of various types of Tuberculosis seen in a cohort of HIV infected children on ART prospectively over a span of mean follow up period of eight (8) years.
Materials and Method: The Institute of Child Health, which is a tertiary care hospital of child care in the heart of the city of Kolkata, catering whole state of West Bengal and neighboring states of Bihar, Odisha, Assam and other north eastern states. Children less than 18 years infected with HIV, presenting with variety of illness and pointing towards immune-deficiency states, were hospitalised. They were tested after voluntary counseling at integrated counseling and testing centre (ICTC) at ICH. Once diagnosis is confirmed, they were referred to centre of excellence for pediatric HIV-AIDS, Medical college, Kolkata for anti-retroviral therapy (ART). Majority of patients co-operated with day to day follow up, taking ART from centre of excellence and rely on us for clinical, immunological and virological follow up. We work in a private clinic at the eastern part of the city where many HIV affected children on regular follow up but the source of ART is from same centre of excellence. If any patient presented with cough and or fever more than 15 days on ART with weight loss or not gaining weight, with or without positive history of contact or any parent died out of HIVTB coinfection, is evaluated for Tuberculosis. The screening tool used here is gastric lavage, sputum for AFB (Acid fast bacilli), Chest X ray, Tuberculin test with 5 TU, Mycobacterial cultutre of specimen like pleural fluid, Cerebrospinal fluid, Pus from cold abscess or lymph node by CBNAAT (Catridge based nucleic acid amplification test) or gene expert. Depending on history, clinical feature and investigation results, anti-TB therapy started by RNTCP DOTs centre or local from market under supervision. Subsequently they were all taken up by DOTS centre.
Results and analysis:
Diagnosis of Tubercular infection in HIV positive children: Due to sharing of a common symtomatology with both HIV and TB infections, many a times we may not be able to detect TB bacilli under standard laboratory method. In HIV infection, extra-pulmonary TB is more common than pulmonary. Hence, smear positivity is much less in advanced stage of the disease. Moreover children less than 7 years can not expectorate sputum. There is a big challenge in convincing our medical colleagues posted at the DOTS centre where they emphasize more on sputum positivity and Tuberculin test. Both can be inconclusive in HIV-TB co-infected children. However in our clinic we follow WHO RNTCP 5 guidelines, for case finding:
Fever and / or cough of recent onset lasting for > 2 weeks arouse suspicion of tuberculosis. (Cough persisting beyond 2 weeks, particularly as an only symptom in an otherwise healthy child can be due to viral infection and is often not due to TB). Recent unexplained loss of weight or not gaining weight for last 3 months . Loss of weight is defined as loss of more than 5% of body weight as compared to highest weight recorded during last 3 months is an important pointer to the suspicion of tuberculosis in our cohort. Radiological picture was given high value in this cohort are hilar or paratreacheal lymphadenitis with or without parenchymal lesion, milliary TB, Tubercular consolidation and secondary pleural effusion. Tubercular skin test (TST) were given high value in TB case finding but negative test i.e.- less than 5mm in HIV patient does not rule out TB as sensitivity is not 100%. History of exposure to an infectious TB patient (Smear positive) always prompted us for detailed examination and intensive history taking for presence of the disease. All efforts were made for sample collection by induced sputum, gastric lavage and microscopy for AFB. Apart from microscopy, all samples were sent for TB culture by CBNAAT.
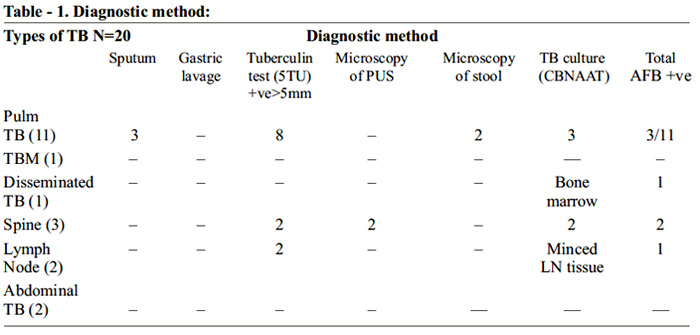
Types of TB and diagnostic method: In this cohort of 20 TB cases, highest number of AFB isolated is Pulmonary TB 3 (15%), followed by spinal cold abscess 2 (10%). AFB was demonstrated in one case of minced cervical Lymph node and Bone marrow culture in disseminated TB. 7 out of 20 HIV TB coinfected children were bacteriologically proven cases (35%). High index of suspicion helped us to reach the diagnosis. In our cohort, sensitivity of Tuberculin test was 60% and it has correlated well with CD4 count. All montoux positivity were observed in high CD4 count of above 500.
TB sites, WHO clinical stage and immunological stage: Contrary to the popular belief that after starting HAART (Highly Affective Anti Retroviral Therapy)6 body recovers its immunological orchestra and opportunistic infection like tuberculosis and others are confined to concentration camp of macrophages and other killer cells. But findings in our cohort emphasizes that TB can happen at any stages of immunological status or recovery and in more than 80% of cases CD 4 count is above 500. PEM is an universal criteria. If present, search for TB.
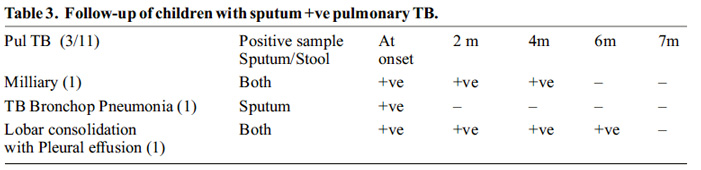
After starting standard four drug Anti TB out of three, two cases of pulmonary TB remained AFB positive even after 4 and 6 months of intensive phase. First case was 10 yrs old boy on ART remains positive for 6 months of intensive phase and negative on seven month. Second case was milliary TB at 11 yrs male on ART remains positive on 4 months sample but negative from 5th onwards.
Conclusion:
In this study, incidence of Tuberculosis is 20% even after enrollment of ART to the tune of 100%, which reminds us that TB can happen at any point of time. There is very small change in the incidence and prevalence of TB in pre and post ART era. Although diagnosis is a challenge to a pediatrician, out of all diagnostic tool Mantoux test is the best indirect test to detect positive cases. It has direct correlation with immunity reflected by CD4 count. All the cases are rifampicin sensitive in our prospective cohort but sputum positivity of two cases even after 4months reemphasizes that shift of intermittent to daily therapy by recent RNTCP guideline is the absolute need of the hour to curb resistance.
References:
1. WHO Global TB report 2016, Tuberculosis fact sheet October 2016.
2. TB India 2016 Revised National TB Control Programme Annual Status Report”, New Delhi, 2016 www.tbcindia.nic.in.
3. WHO Global TB repoprt 2013.
4. Zar HJ, Hanslo D, Apolles P, Swingler G, Hussey G. Induced sputum versus gastric lavage for microbiological confi rmation of pulmonary tuberculosis in infants and young children: a prospective study. Lancet 2005; 365: 130–34.
Issue: January-March 2017 [Volume 6.1]
