Fulminant Hepatitis A Infection In A Child With Insulin Dependent Diabetes Mellitus
Case Report
Corresponding author: Dr Revathi N, Associate Professor ,Department of Pediatrics, MGM Hospital and Medical College, Kamothe, Navi Mumbai, Maharashtra, India.
Email: nrevati@rediffmail.com Telephone no: 919969628043
Received: 22 th March, 2019; Reviewed: 11th June, 2019; Accepted :29th June ,2019.
Citation of article: Revathi N, Priyanka S Amonkar,Vikram S Patra,Jeetendra Gavhane,Bageshree Seth .Fulminant Hepatitis A Infection In A Child With Insulin Dependent Diabetes Mellitus .New Indian Journal of Pediatrics,2019; 8.2:
Abstract: Diabetes mellitus (DM) is known to complicate liver diseases like hepatitis. A 13-year-old boy was brought to the hospital with fever, jaundice, high coloured urine for five days and lethargy. There was tender hepatomegaly with a liver span of 12 centimetre .The child was admitted in paediatric intensive care unit with a provisional diagnosis of viral hepatitis with encephalopathy.The blood sugar was 225 mg/dl on admission. One week after discharge, the child presented with increased intensity of jaundice, abdominal pain, pruritis and high coloured urine. On examination, there was a weight loss of 2 kilograms and deep icterus.His blood sugars were abnormal (fasting 425mg/dl; post prandial 633 mg/dl). The pancreatic enzymes were normal.HbA1C level was 10.4 which suggested that the child probably had altered glucose metabolism before the episode of acute viral hepatitis. The jaundice resolved after a brief period of cholestasis and the child is now on regular follow-up for Type-1 diabetes for the past one year.
Keywords: Fulminant Hepatitis, Insulin Dependent Diabetes Mellitus, cholestatic jaundice.
Introduction: The interaction between diabetes and infection is complex. The disease itself predisposes an individual to infections. Liver being the major site of glucose metabolism, abnormal glucose homeostasis can occur as a complication of liver diseases like hepatitis, cirrhosis and fulminant hepatic failure [1]. Also, diabetes mellitus (DM) is known to complicate liver diseases like hepatitis. We present a rare case of complicated hepatitis A infection in a child with insulin dependent diabetes mellitus (IDDM). One week after discharge, the child presented with increased intensity of jaundice, abdominal pain, pruritis and high coloured urine.
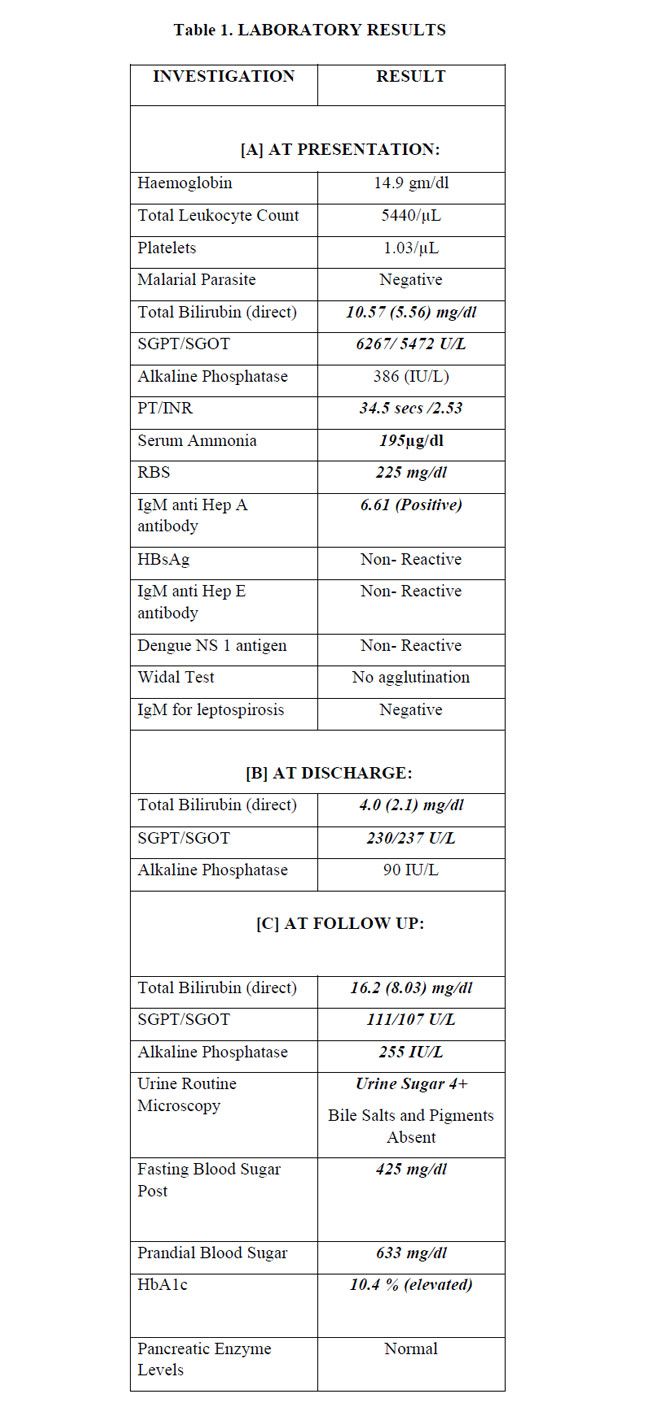
Case report: A 13-year-old boy was brought to the hospital in a confused state with irrelevant speech. He had fever, jaundice and high coloured urine for five days. Physical examination showed stable vital parameters with a GCS of 13/15. Abdomen was soft. There was tender hepatomegaly with a liver span of 12 centimetreand no splenomegaly. There was no ascites or bleeding manifestation. The child was admitted in paediatric intensive care unit with a provisional diagnosis of viral hepatitis with encephalopathy.The blood sugar was 225 mg/dl on admission. The child was started on appropriate management for hepatic encephalopathy and was simultaneously investigated for aetiology(Table 1A). IgM anti- Hepatitis A antibody level was found to be positive (6.61). Except for one episode of hypoglycaemia, the blood sugar levels were maintained between 150 mg/dl and 200 mg/dl on Glucose Infusion Rate (GIR) of 4 throughout his PICU stay, which lasted for 3 days. He was discharged after clinical and lab improvement (Table 1B).
One week after discharge, the child presented with increased intensity of jaundice, abdominal pain, pruritis and high coloured urine. On examination, there was a weight loss of 2 kilograms and deep icterus. Per abdominal examination revealed mild hepatomegaly. On investigation, (Table 1[C]) he had cholestatic type of jaundice and was treated as post infectious cholestatic jaundice. As the child had weight loss despite normal appetite, we simultaneously investigated him for the same and found that blood sugars were abnormal (fasting 425mg/dl; post prandial 633 mg/dl). The pancreatic enzymes were normal.HbA1C level was 10.4 which suggested that the child probably had altered glucose metabolism before the episode of acute viral hepatitis. He was started on insulin and was sent home after titration of dose. The jaundice resolved after a brief period of cholestasis and the child is now on regular follow-up for Type-1 diabetes for the past one year.
Discussion:The interaction between viral infections and IDDM has been analysed in detail by Filipi et al [2]. This analysis, which is based on epidemiology, clinical investigations and experimental work, suggests that the relationship between IDDM and viral infection is complex. A significant number of viruses like coxsackievirus B, rotavirus, mumps virus, cytomegalovirus and rubella virus (congenital infection) have been found to promote autoimmunity, thereby causing IDDM. Hepatitis virus and IDDM co-existence as an association or as causative factor has been reported in adults, especially with respect to Hepatitis B and Hepatitis C related chronic liver disease [3]. Hepatitis C has been found to have a causative role in diabetes [3-6].Hepatitis A, which usually results in a self-limited acute infection of theliver, has been reported to have caused diabetes mellitus in adult population during an epidemic of infectious hepatitis in Nigeriaas early as 1976 [7].However, diabetes in all the cases of hepatitis A during the epidemic resolved completely after a few months.There are reports of fulminant IDDM following hepatitis A infection from South Korea and India [8,9].So far, there is only one report of Hepatitis A infection in child with pre-existing IDDM [10]. The infection in this case resolved without any complications.
In our child, the presentation of Hepatitis A was very severe and he developed another uncommon complication of hepatitis A, which is cholestatic jaundice. [11] The diagnosis of IDDM was made during the convalescence period. The elevated HbA1c indicated that he had altered glucose levels even before the onset of hepatitis A infection which may have resulted in a more fulminant course. Hypoglycaemia is a known complication of hepatic failure and probably concealed the effect of IDDM. This is the first case report of fulminant hepatitis A infection unmasking underlying IDDM.
Conclusion: Hepatitis A infection is usually self-limited. Underlying IDDM probably resulted in a more fulminant course of the disease in this case. The above fact underscores the need to vaccinate children with IDDM against Hepatitis A and possibly other vaccine preventable diseases.
Key Message: There is need to vaccinate children with diabetes mellitus which is immunodefficiency state.
Conflict of interest: None
Funding: None
References:
1) Levinthal GN, Tavill AS. Liver disease and diabetes mellitus. Clinical Diabetes [serial on line].1999; 17(2). Available at: www.journal.diabetes.org/clinicaldiabetes
2) Filippi CM, Von Herrath MG. Viral Trigger for Type 1 Diabetes: Pros and Cons. Diabetes. 2008;57(11):2863-2871.
3) Ryu JK, Lee SB, Hong SJ, Lee S. Association of Chronic Hepatitis C Virus Infection and Diabetes Mellitus in Korean Patients. The Korean Journal of Internal Medicine. 2001;16(1):18-23.
4) Allison ME, Wreghitt T, Palmer CR, Alexander GJ. Evidence for a link between hepatitis C virus infection and diabetes mellitus in a cirrhotic population. J Hepatol. 1994;21:1135-39. 5) Ozyilkan E, Arslan M. Increased prevalence of diabetes mellitus in patients with chronic hepatitis C virus infection. Am J Gastroenterol.1996;91:1480-81. 6) Gray H, Wregitt T, Stratton IM, Alexander GJ, Turner RC, O’Rahilly S. High prevalence of hepatitis C infection in Afro-Caribbean patients with type 2 diabetes and abnormal liver function tests. Diabetic Med.1995;12:244-49.
7) Adi FC. Diabetes Mellitus Associated With Epidemic Of Infectious Hepatitis In Nigeria.The British Medical Journal.1974;1(5900):183–185.
8) Hwang YC, Jeong IK, Chon S, Oh S, Ahn KJ, Chung HY, et al. Fulminant Type 1 diabetes mellitus associated with acute hepatitis A. Diabetic Medicine. 2010;27: 366–367. 9) Ali N, Veetil VM, Vijayan AP, et al.Fulminant type 1 diabetes occurring in a child in association with acute hepatitis A infection: case report and review of literature. Int J Diabetes Dev Ctries. 2016;36: 374.
10) Hasosah M, Bokhari A, Alsahafi A, Sukkar G, Alzaben A. A Rare Association of Hepatitis A Virus Infection with Type-1 Diabetes. Clinics and Practice. 2016;6(2):844.
11) Arief S, Hernik R, Nugrohowidhi A, Hidayat B. A Cholestatic Type of Hepatitis A in a Child. Paediatr Indones.2001;41:308–10.
Issue: April – June 2019 [Volume 8.2]