Reappraisal of Gastric Aspirate Cytology as a Screening Tool for Neonatal Sepsis in Very Low Birth Weight Babies
Original Research
Abstract:
Aims and objectives: To assess the role of Gastric aspirate cytology as marker for Neonatal sepsis in Very low birth weight babies. We compared gastric aspirate cytology and blood culture of the babies and high vaginal swab of the respective mothers, in a group of VLBW babies. Settings: Special care nursery of a multi speciality teaching and regional referral hospital in West Bengal, India. Study Design: Case Control study. Participants: 150 VLBW babies were selected randomly. Out of them 55 babies were suffering from neonatal sepsis (cases) and remaining 95 were clinically normal (Controls). Interventions: Gastric aspirate cytology done for the babies (n = 150) Blood culture done for the babies (n = 150) High vaginal Swab for culture of the mothers of the above mentioned babies (n = 150). Sepsis screen done for the babies (n=150).
Main outcome measures:
Association between the incidence of sepsis, gastric aspirate cytology and high vaginal swab results.
Results:
It is seen there is strong association between neonatal sepsis, especially early onset sepsis, positivity of maternal high vaginal swab and positive gastric aspirate cytology in VLBW babies. Results were tested against controls with Chisquare test and significance of association was obtained.
Conclusion:
Gastric aspirate cytology is an inexpensive and specific marker for early determination of risk of neonatal sepsis in VLBW babies. It can be an indispensable part of any sepsis screen.
Key Words:
VLBW babies, Neonatal sepsis, Gastric aspirate cytology.
Introduction:
Neonatal sepsis and prematurity are collectively taken as the greatest killer of neonates in India and also worldwide (1, 2). In Early onset Neonatal sepsis (EOS) that occurs within 72 hours of age the infection is mainly acquired either antenatally or during intranatal events (3). Risk factors that are known to be associated to its occurrence are prelabour rupture of membranes, more than three internal examinations, maternal fever, chorioamnionitis and foul smelling liquor (4). Microbiological examination of the maternal high vaginal swab (HVS) may also act as risk factor assessment tool for neonatal sepsis, mainly of the EOS variety. Late onset sepsis (LOS) occurs after 72 hours and mainly acquired postnataliy.
VLBW babies are mostly premature, and are 3 to 10 times more susceptible to sepsis than term babies due to lack of immunity, increased occurrence of respiratory distress syndrome and necrotising enterocolitis, and multiple interventions that are required for their survival (5). The overall incidence of neonatal sepsis in VLBW babies is 10 to 30 per 1000 live births. Early diagnosis of sepsis in these babies improves their survival rate. The clinical picture due to prematurity often masks the typical presentations of neonatal sepsis in these babies; creating a diagnostic dilemma. Diagnosis of neonatal sepsis requires a high clinical suspicion, and the of presence of thee or more risk factors or foul smelling liquor or two risk factors with positive sepsis screen performed by various indirect methods , and confirmation by blood culture, pertains to a diagnosis of sepsis . However, as blood culture being positive in only 39.7% of the clinical cases, one has to rely on other parameters, perhaps sepsis screen, for diagnosis (6). Considering the high burden of disease VLBW babies very often needs sepsis screen. In India, National Neonatology Forum (NNF) has forwarded a protocol comprising of total leucocyte count, Creactive protein, ratio of immature to total neutrophil count, micro ESR and absolute neutrophil count for screening of sepsis in all babies. And when two or more of them are positive then it is considered as clinical or probable sepsis (7), and are considered as cases and needs antimicrobial therapy. There are various other sepsis screens used in other parts of the world such as the haematological scoring system (HSS) by Rodwell et al., HSS with haptoglobin as by Philip (1980) and many others. Many of them have high sensitivity and specificity as well, and are useful in diagnosing neonatal sepsis in these babies (8). Gastric aspirate cytology is an age old and inexpensive technique mostly used as a risk factor assessment tool, indicating exposure to intrauterine infection (9). It can be done in a peripheral setting and as it is done prior to first feed of the baby, an early assessment can be obtained.
The present study has tried to establish Gastric aspirate cytology as a marker for neonatal sepsis in VLBW babies.
Methods:
This is a case-control study conducted at the Special care nursery of a multi speciality teaching and regional referral hospital in West Bengal, India, namely Burdwan Medical College; from April 2014 to March 2015; after approval from the Ethical committee of the institution. The study included 150 VLBW babies that were selected randomly, and babies born with congenital anomalies, asphyxiated or with any metabolic disorders were excluded from the study. Gastric aspiration done with infant feeding tube of 5- 6 Fr prior to first feeding and preferably 1 hour after birth, followed by smear preparation and cytology, were done for all babies at our SCNU side lab. Presence of more than 5 polymorphs per high power field or more than 75 % polymorphs to epithelial ratio was taken ‘positive’ (3). Blood culture was done for all the babies prior to antibiotic therapy. Aseptically drawn 0.5 to 1.0 ml of blood from fresh venesection sites were placed in standard soy broth culture bottle; and incubated for up to 5 days through modern culture techniques (BACTEC). High vaginal swabs were taken from mothers of all these babies and cultured. Sepsis screen, as per the NNF protocol, were done for all the babies. As per Mouzinho’s chart higher limit for normal I/T ratio was taken as 1.6 (10). Ethical committee of the institution reviewed the topic and methods, and approved the study. Proper consent was taken from the parents or guardians of all these babies prior conducting the study.
Data analysis:
The data being categorical were analysed using Chi-square (?2) test to measure the significance of association between the various categories. Relative risk, odds ratio, sensitivity, specificity and predictive values were also determined. SPSS 17.0 software was used to analyse the data.
Results:
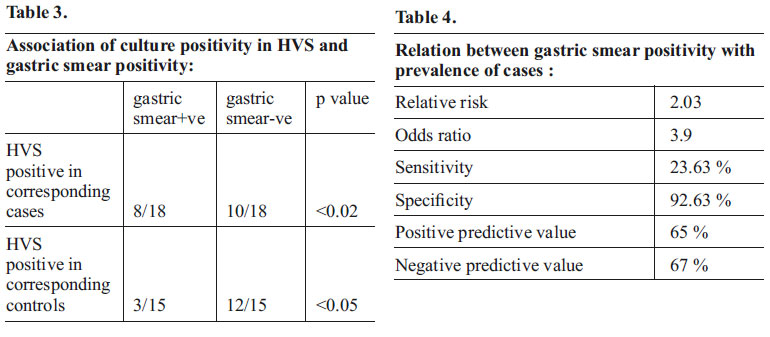
During the study period, 150 VLBW babies were randomly selected for the study. The mean birth weight and mean gestational age were 1243 grams and 32 weeks respectively (table 1). Sex ratio in case group is 1:1, and control group is 1.3:1. Babies with neonatal sepsis (n=55) presented with poor feeding (66.7% of EOS and 9.8% of LOS), tachypnoea (83.3 % of EOS and 21.4 % of LOS), cyanosis (61.1% of EOS and 35.7% of LOS), hypothermia (50.0% of EOS and 21.4 % of LOS), apnoea (27.8% of EOS and 14.3% of LOS), convulsions (11.1% of EOS and 42.8% of LOS), and abdominal distension (11.1% of EOS and 21.4% of LOS). Out of the 55 babies with sepsis 55 % had positive CPR, 41% had raised microESR (>15 mm in first hour), 12 % had leucopenia (TLC<5000/cmm), 15% had neuropenia (ANC < 1500/cmm), and 28% of babies had bandaemia (band cell count >16% of total neutrophils). And, 45 babies among the 55 cases were found to have 2 or more than 2 screen factors positive (ie: screen positive cases). Blood cultures were positive in 20 babies, designated as ‘culture proven’ cases of sepsis. The organisms isolated were E.coli (n=8, 40%), S. aureus (n=5, 25%), Klebsiella sp. (n=4, 20%), coagulase negative Staphylococci (n=2, 10%), and Pseudomonas (n=1, 5%). The remainder 95 VLBW babies, which were neither found to have clinical (rather screen positive) sepsis or culture proven sepsis, and were taken as controls. Table no. 2 shows Gastric smear analysis was found to be positive in 13 out of 55 cases and in only 7 out of 95 controls; and the correlation was found to be significant (p value <0.01). It also shows the relation of gastric smear analysis with the two types of sepsis. Gastric smear analysis was found to be positive in 10 of the 19 EOS cases (52.6%), and in 3 of the 36 LOS cases (8.33%); and it was found to be highly related to EOS ( p value < 0.001). Table no.3 shows association between culture positivity in Maternal High Vaginal Swab study (HVS) and gastric smear positivity. Among the 18 cases found to have culture positive HVS, 8 were having positive gastric smears (44%); while it was only 5 gastric smear positive cases out of 37 HVS negative cases (13.5%). Also in the control group 3 found gastric smear positive among the15 HVS positive group (20%), and 4 found gastric smear positive among the 80 HVS negative group (5%). Association was significant in both the case group (p value <0.02) as well as in the control group (p value <0.05). Table 4 enumerates the various statistical outcomes of the study. An Odds ratio of 3.9 and a positive predictive value of 65 % are encouraging figures.

Discussion:
In the present study, the significance of association of gastric aspirate cytology with the prevalence of neonatal sepsis is less than 0.01. Much better association has been noted with culture proven sepsis and EOS (both having p values less than 0.001). The maternal high vaginal swab studied for culture positivity, which merely suggests presence of high load of birth canal flora, showed a good association with the number of gastric smear positive subjects both in case group (p <0.02) and in control group (p <0.05). This data analysis reiterated the fact that, positive gastric aspirate cytology signifies exposure to intrauterine infection, and that EOS is mainly acquired from maternal genital tract infections, chorioamnionitis or mere high load of birth canal flora without any clinical manifestations in her (11)
The present study deduced an odds ratio of 3.9 with a positive predictive value of 65 % indicating it as a good tool to assess risk of sepsis in a neonate. A very high specificity (92.63 %) makes it an important tool to rule out exposure to intrauterine infections and thus to exclude the risk of EOS. However, present data describes the test as having low sensitivity (23.63 %). Presently sepsis screen consists of CRP, TLC, ANC, and ESR; and collectively their sensitivity and specificity are 56 and 94 respectively. Anita Chandna, M. Nagaraj Rao, M. Srinivas and S. Shyamala from the Department of Paediatrics, Gandhi Medical College, Hyderabad, India have shown that if Gastric aspirate cytology is done along with CRP then the sensitivity rises to 83%, specificity is 76% and the positive predictive value is 48% (12). Hence gastric aspirate cytology can be used with other screening tools to collectively increase its sensitivity.
Conclusion:
India is a large country and about one million VLBW babies are born every year, so the burden of disease is very high. Gastric aspirate cytology is an inexpensive tool, requires very little infrastructure, and can be arranged in a rural setting. And if it is incorporated in sepsis screen more and more babies can avail better patient care. This will also reduce indiscriminate use of antibiotics on normal VLBW babies who are only sick by virtue of their prematurity. Previous studies have established the fact for newborns of all birth weight categories.
What the study adds :
The present study has focussed only on VLBW babies, and has tried to establish the same in that birth weight category. This hypothesis could be operational in other countries too. However there is always a scope and requisite for further research to strengthen the above in the given and other geographical and demographical locations.
Grants / Funding:
None required, as the study was conducted at a Government run Hospital.
Competing Interest:
None found.
Role of authors:
Roy Atanu*-Data collection, analysis and writup.
Ghosh Tarak Nath*, Datta Asok Kumar**- Concept, design and supervision. Barik Kanai Lal**, & Chaudhary Nabendu# – supervision and editing
References:
1. Report of National Neonatal Perinatal Database, 2002-03. National Neonatology Forum, www.jnnfi.org.
2. Puopolo Karen N. Epidemiology of Neonatal early onset sepsis. Neoreviews. 2008: 9: e571- e579.[ http://neoreviews.aappublications.org /cgi/content/full/neoreviews;9/12/e571].
3. ‘Neonatal Sepsis’. Paul V, Aggarwal R. Manual of Neonatal Care; Mondkar J, Pejaver RK (eds); National Neonatology Forum. Prism Books, Bangalore; 2004.
4. Schuchat A et al : Risk factors and opportunities for prevention of early –onset neonatal sepsis. A multicentre case – control study. Paediatrics, 105: 21.
5. Lewis DB, Wilson CB: Developmental Immunology & role of host defences in neonatal susceptibility to infections. In: Remington JS, Klein JO (eds.), Infections of Foetus and Newborn Infant; 4th ed. Philadelphia, WB Saunders, 1995: 20- 98.
6. Thakre R. Neonatal sepsis screen. Pediatrics Today; vol. VIII no. 3: 176.
7. Sankar M, Aggarwal R, Deorari A.K. and Paul V. K. ‘Sepsis in the newborn’ , Indian J Paediatr. 2008; 75: 261 – 266.
8. Rodwell RL, Taylor KM, Tudehope DI, Gray PH. Hematologic scoring system in early diagnosis of sepsis in neutropenic newborns. Pediatr Infect Dis J. 1993 May;12(5):372-6..
9. Thomas S, Verma I. C, Singh M, Ghai O. P. and. Parida S. N. ‘Rupture of membranes, gastric aspirate cytology and neonatal sepsis’. Indian J Paediatr; 47: 511-514.
10. P.Ferreira, T.Bunch, K.Albertine, D.Carlton. Circulating neutrophil concentration and respiratory distress in premature infants. J Pediatrics; 136, Issue 4: 466-472
11. Vasan U, Lim D M, Greenstein RN, Raye JR, Origin of gastric aspirate Polymorphonuclear cells in infants born after prelabor rupture of membranes. J. Pediatr ; 47: 735 – 40.
12. Chandna A, Nagaraj Rao M, Srinivas M and Shyamala S. Rapid diagnostic tests in neonatal septicaemia. Indian J Paediatr; 55: 947 – 953.
Issue: January-March 2016 [Volume 5.1]
