Clinical Pattern and Malnutrition among Children with Congenital Heart Disease (CHD) Attending Two Centres Under the RBSK Scheme
ORIGINAL RESEARCH
SreeMookambika Institute of Medical Sciences, Kulasekharam. Kanyakumari, Tamil Nadu & SAT Hospital, Government Medical College, Thiruvananthapuram, Kerala, India-695011
RECEIVED:13 TH July,2018 REVIEWED:12TH October 2018, ACCEPTED:19 th December 2018
Correspondence: Dr. Elizabeth K E, Mangalathumannil, Nalanchira, Thiruvananthapuram, Kerala, India -695015, drelizake@gmail.com
Received: 23 th August,2018; Reviewed:24th October 2018, Accepted:21 th December 2018
Citation Of Article: Elizabeth K. E., Nargis Rabiya., Geetha V Clinical Pattern and Malnutrition among Children with Congenital Heart Disease (CHD) Attending Two Centres Under the RBSK Scheme
ABSTRACT: Introduction: Congenital Heart Disease (CHD) is the most common congenital anomaly in children requiring intervention for survival and quality of survival. The time and type of intervention and the nutritional status of the children are key determining factors of outcome. As per the prevalence, available resources and health seeking behavior, the clinical profile and nutritional status of CHD is likely to vary from centre to centre. The Rashtriya Bal SwasthKaryakram (RBSK) Scheme was launched in India in 2013 to address the 4D’s; defects, deficiencies, diseases and developmental delay & disability among 0-18-year-old children.
Objective: To compare the clinical profile and nutritional status of children with CHD admitted to two tertiary care teaching institutions, under the RBSK Scheme.
Methods: Consecutive cases with Acyanotic CHD (ACHD) and Cyanotic CHD (CCHD) admitted to SAT Hospital, Govt. Medical College, Thiruvanathapuram, Kerala, India (Centre A) and SreeMookambika Institute of Medical Sciences, Kulasekharam. Kanyakumari, Tamil Nadu (Centre B), were evaluated for type of CHD and nutritional status and socio-demographic data.
Results: The children attending the government facility in Kerala (Centre A) were mostly in born babies or referred from other hospitals. The children attending the private facility in Tamil Nadu (Centre B) were referred from camps and school health programs. The socio-economic status was comparable, and majority belonged to middle and lower class.The male to female ratio was comparable. In the government facility in Kerala, there were more infants less than 1 year of age where as in center B majority were above 1 year of age. In both centers, majority were underweight and had varying grades of stunting and wasting, indicating chronic and acute malnutrition respectively. Stunting was more in children with CCHD, with chronic hypoxia. ACHD was more, compared to CCHD, in both centers. Among ACHDs, VSD was more in Center A and ASD was more in Center B. Among CCHD, Tetralogy of Fallot (TOF) was more common in both centres.
Conclusion: There was significant difference in the age group and clinical pattern among the children with CHD, attending the two centers under the RBSK scheme, as per the referral pattern. Socio-economic status and male to female ratio were comparable. Majority were underweight, stunted and wasted, indicating both chronic and acute malnutrition, which is a known determinant of poor outcome. ACHD was more common than CCHD and VSD was more common in the early referral group and ASD in the late referral group. This comparative study is presented in view of its public health importance.
INTRODUCTION: The prevalence of congenital heart disease (CHD) varies from 0.6 to 9 per thousand live births and accounts for one third of all birth defects (1). The prevalence varies based on the available diagnostic facilities. In India, the prevalence of CHD is reported to be 2.25 to 5.2 per 1000 live births(2).The etiology of CHD is multifactorial; ranging from chromosomalor monogenic defects, environmental factors like teratogens to maternal diseases like diabetes mellitus. The burden of CHD is high in developing countries like India, due to the high birth rate and critical nature of CHD requiring expensive surgical and non-surgical interventions.
Rashtriya Bal Swasthya Karyakram (RBSK) scheme was launched in India to address the 4 Ds; defects at birth, deficiencies, diseases and developmental delay &disabilities (3). This scheme is a big boon to the society, as it addresses many public health issues including the burden of CHD. Both government and private institutions are accredited to undertake interventions under this scheme. However, the pattern of CHDs, the nutritional status of children and health seeking behavior may vary from region to region. Hence, a study was undertaken to compare the pattern of nutrition status of children with CHD attending a government facility in Thiruvananthapuram district of Kerala state and a private facility in Kanyakumari district of Tamil Nadu state.
MATERIALS AND METHODS: All consecutive cases of heart diseases admitted to pediatric ward in the 2 centers for six months period, during 2015- 2016 were enrolled. Centre A was Sree Avittom ThirunalHospital (SATH),Government Medical College, Thiruvananthapuram from Kerala state. Centre A is not a cardiac intervention entre, but due to its proximity to Sree Chitra Thirunal Institute of Medical Sciences (SCTIMST), had the advantage of easy referral for immediate intervention. Centre B was Sree Mookambika Institute of Medical Sciences (SMIMS),Kulasekharam, Kanyakumari district from Tamil Nadu state. Centre B is a cardiac intervention centre, where the government scheme was available for intervention. Socio demographic data and dietary profile were collected using a structured proforma. Anthropometric measurements were done using standard equipment’s and procedures, ensuring intra-observer reliability (4). Nutritional status like weight for age, height for age, weight for height was compared with IAP growth charts (5). Socio-economic status was assessed using Modified Kuppuswamy scale (6).Institutional Ethic Committee approval and parental consent were taken prior to enrolment in the study. Cardiac evaluation was done using X-Ray Chest, ECG and Echocardiogram, undertaken by Paediatric Cardiologist. Analysis of data was done using SPSS version 16.
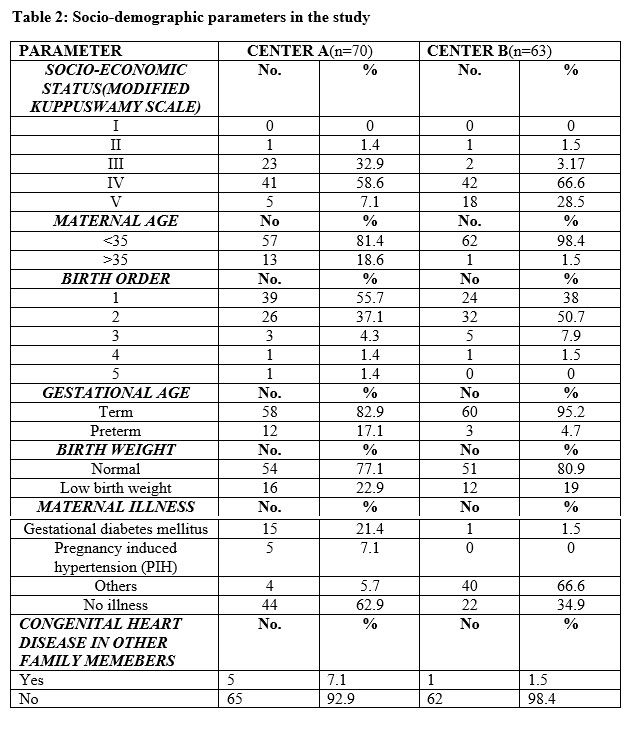
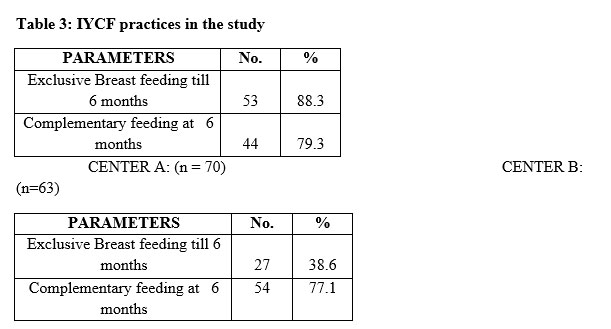
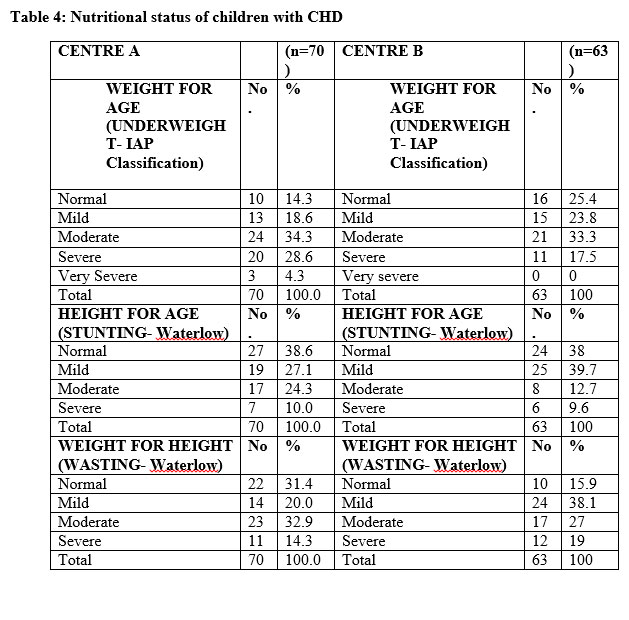
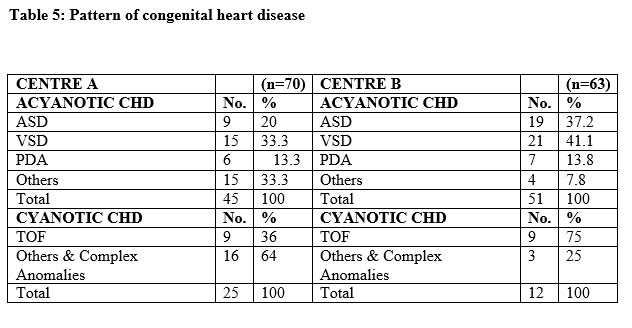
RESULTS: 70 children were enrolled in center A and 63 children in center B, during the study period of six months. The distribution of children according to age and sex are givenin table 1. Infants less than 1 year were more in Center A compared toCenter B. The male to female ratio in Center A was 1:1 and Center B was 1:0.9 and was comparable (P > 0.05). The Socio demographic parameters are summarized in table 2. Majority, who were enrolled under the scheme, belonged to low socio-economic status in both the centers. Comparison of the Infant and young child feeding (IYCF) practices among the children are given in table 3. In both centers, most of the children were underweight and had varying grades of stunting and wasting, indicating chronic and acute malnutrition respectively. Comparison of the nutritional status among the children is given in table 4.Acyanotic congenital heart disease (ACHD) was more, compared to Cyanotic Congenital Heart Disease (CCHD), in both centers. Among ACHDs, VSD was more in Center A and ASD was more in Center B. Among CCHD, Tetralogy of Fallot (TOF) was more common in both centers. The pattern of CHD and the proportion of ACHD and CCHD are given in table 5.
DISCUSSION: The number of children enrolled in Center A and Center B, during the study period, was comparable (70 vs. 63). The children attending the government facility in Kerala (Centre A) were mostly inborn babies or referred from other hospitals. The children attending the private facility in Tamil Nadu (Centre B) were referred from camps and school health programs. The difference in the referral pattern was due to the fact that Center A is a tertiary care teaching hospital with proximity to a National Institute(SCTIMST)) catering to critical heart disease and Center B is a tertiary care teaching hospital, which has a cardiac intervention center undertaking both surgical and non-surgical procedures.
In the government facility in Kerala, there were more infants less than 1 year of age where as in center B majority were above 1 year of age. This difference in distribution of age of children was statistically significant (p<0.0.5). This difference is due to the difference in referral pattern in the two centers. The male to female ratio was comparable in both centers (1:1 vs 1:0.9). This is in accordance with the study done on gender equality of children with CHD in 2011 (7). However, another previous study in Kathmandu had reported a ratio of 1.5:1. Gender equality noted in both the centers in the present study is encouraging.
Majority belonged to lower middle and lower class, as per modified Kuppuswamy scale (Class III, IV) except for one child eachfrom both centers, who belonged to the upper middle class II. This reflects the health seeking behavior under the government schemes like RBSK and may also be due the higher prevalence of CHD among those belonging to lower socio-economic status.A previous study had suggested that the prevalence of CHD is more among children belonging to low socio-economic status (8).
In 18.5% cases, maternal age was more than 35 years at conception in Center A, which is a large maternity centre catering to high risk mothers. It was only 1.5% in Center B. This difference is attributable to the referral pattern in the two settings. Even though chromosomal anomalies in off springs may occur more in elderly mothers, CHD is reported to occur independent of the maternal age (9). In center A, 55.7% belonged to birth order one compared to 38% in Center B. Being the first born is reported as an independent risk factor for occurrence of CHD (10). However, an Indian study had reported that the risk for CHD increases as birth order increases to more than two (11).
Majority in both the centers were born as term babies. 22.9 % in Center A and 19% in Center B were born as low birth weight babies. In Center A 21.4% gave history of gestational diabetes mellitus (GDM), 2.97 % had GDM and pregnancy induced hypertension (PIH) and 5.9% had other illness like hyperemesis gravidarum. In Center B, 1.5% gave history of GDM and 66.6% had other illness like hyperemesis gravidarum. Maternal illnesses, especially GDM are a known risk factor for development of CHD (12). In Center A, 7.1% gave history of CHD in other family members and in Center B, 1.5% had CHD in other family members. Familial cases of CHD due to monogenic inheritance had been reported (13).Majority of cases of CHD show multi factorial inheritance.
Exclusive breast feeding till six months of age was reported among 38.6% in Center A compared to 88.3% in Center B. This may be due to the urban rural differences in the catchment areas of the two centres. The introduction of complementary feeding at 6 months of age was comparable in both the centers. Early cessation of breast feeding and early as well as late introduction of complementary feeding is known risk factors for malnutrition in children with CHD (14).
Malnutrition is often the rule in children with CHD. The type of cardiac anomaly is known to influence the nutritional status. Dietary inadequacy and the disease burden contribute to malnutrition. Early nutrition screening and intervention is recommended in children with CHD for better outcome (15, 16). Various studies had reported high prevalence of malnutrition in children with CHD (17). 85.8% in Center A and 74.6% in Center B were underweight and 4.3% in Center A were severely underweight. (18). The proportion of underweight children was comparable in ACHD and CCHD. Majority, 61.4% in Center A and 62.0% in Center B had varying grades of stunting, indicating chronic malnutrition. Stunting was more in those with CCHD, in accordance with the previous report by Varan et al. (18). This is attributable to the chronic hypoxia in children with CCHD. Majority, 67.2% in Center A and 84.1% in Center B had varying grades of wasting, indicating acute malnutrition. This finding is similar to other reported studies (19).
Comparison of IYCF practices and nutritional status of children with CHD in the two centres with NFHS -4, 2015-16 data (20), and showed significant differences. Exclusive breastfeeding during first six months was 46.4% compared to 38.6% in Centre A to 88.3% in Centre B. Six-month-old receiving solids/semisolids and breast milk was 52.6%, compared to over 70% among those with CHD in both centres. 42.5% were underweight, but children with CHD were more underweight, 85.8% and 74.6% respectively. 48% were stunted compared to 61.4% and 62% respectively among children with CHD. 19.8% were wasted compared to 67.2% and 84.1%, respectively in the present study. Those with severe wasting were 14.3% and 19% respectively in the present study compared to 6.4% as per NFHS data (20). Poor nutritional status is a known determinant of adverse outcome in children with CHD.
ACHD is more common than CCHD. Among ACHDs, ventricular septal defect (VSD) is the most common heart disease in children and PDA in newborn babies. Majority, 71.4% in Centre A and 18.9% in Center B had ACHD. VSD was more common in Center A and ASD in Center B. ASD is usually diagnosed in older children due to the late onset of symptoms. Among CCHD, TOF was the most common in both centers, as expected. The difference in the pattern of CHDs in both the centers is attributable to the referral bias and difference in the age group of the participants. Centre A had more your children, referred from hospitals and Centre B had more older children, referred from camps and school screening programmes. Screening under the RBSK Scheme is a good initiative, especially for those belonging to low socio-economic status.
CONCLUSION: There was significant difference in the age group, clinical pattern among the children with CHD, attending the two centers under the RBSK scheme, as per the referral pattern. There was no gender difference in the children seeking medical care under the scheme. All except one child in each centre, belonged to the low socio-economic status. Majority were underweight, stunted and wasted, indicating both chronic and acute malnutrition, which is a known determinant of poor outcome. Stunting was more in children with CCHD, with chronic hypoxia. ACHD was more common than CCHD and VSD was more common in the early referral group and ASD in the late referral group. The findings of the study throw light on the regional differences in clinical profile, nutritional status and the referral pattern of children with CHD. Addressing the backlog of cases with CHD is expected to result in early intervention in all newly diagnosed cases in the future. The RBSK scheme was noted as a big boon to children with CHD, especially belonging to low socio-economic status.
DECLARATIONS: Contribution of authors: – Elizabeth K. E -concept ,strategy, guidance, , Nargis Rabiya – supervision and revision of manuscript, Geetha V -data collection,statistical analysis,,initial manuscript,
Funding: None
Conflict of interest: None
Ethical approval: Approved by hospital ethical committee
References:
1. Van der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ, Roos-Hesselink JW. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am CollCardiol. 2011;58:2241-47. doi:10.1016/j.jacc.2011.08.025.
2. Anita S.Congenital Heart Disease in India: A Status Report. Indian J Pediatr. 2005; 72: 595-98
3, Gupta A, Kumar R, Khera A, Sankar S, Khurmi M, Srivastava A, et al. Operational Guidelines Rashtriya Bal SwasthyaKaryakram. 2012
4. WHO Working Group. Use and interpretation of anthropometric indicators of nutritional status. Bull WHO 1986, 64: 927- 941
5. Khadilkar VV, Khadilkar AV. Revised Indian Academy of Pediatrics 2015 growth charts for height, weight and body mass index for 5–18-year-old Indian children. Indian J Endocrinol Metab 2015; 19(4):470–6.
6. Mishra D, Singh H. Kuppuswamy socio-economic staus scale- A revision. Indian J Pediatr. 2003, 70: 273-274
7. Singh D, Wander GS, Singh RJ. Gender equality in India for children with congenital heart disease: looking for answers. Heart 2011;97(23):1897-8.
8. Mughal AR, Sadiq M, Hyder SN, Qureshi AU, A Shah SS, Khan MA, Nasir JA. Socioeconomic status and impact of treatment on families of children with congenital heart disease. J Coll Physicians Surg Pak 2011;21(7):398-402.
9. Best KE, Rankin J. Is advanced maternal age a risk factor for congenital heart disease? Birth Defects Res A Clin Mol Teratol 2016;106(6):461-7.
10. Nora JJ, Nora AH. The Environmental Contribution to Congenital Heart Disease. In: Nora, J.J. and A. Takao (Eds.), Congenital Heart Disease: Causes and Processes. Future Publishing Co., Mount Kisko, New York, 1984. pp: 15-2
11.Rothman KJ, Fyler DC. Sex, birth order and maternal age characteristics of infants with CHD. Am J Epidemiol 1976;104: 527-34.
12.Wren C, Birrell G, Hawthrone G. Cardiovascular malformation in infants of diabetic mothers. Heart. 2003; 89: 1214-1220.
13. Oyen N, Poulsen G, Boyd HA, Wohlfahrt J, Jensen PKA, Melbye M. Recurrence of Congenital Heart Defects in Families. Circulation. 2009;120:295-301
14. Okoromah CAN, Ekure EN, Lesi FEA, Okunowo WO, Tijani BO, Okeiyi JC. Prevalence, profile and predictors of malnutrition in children with congenital heart defects: a case–control observational study. Arch Dis Child 2011 Apr 1; 96(4): 354-60.
15. Vaidyanathan B, Nair SB, Sundaram KR, Babu UK, Shivaprakasha K, Rao SG, Kumar RK. Malnutrition in children with congenital heart disease (CHD) determinants and short term impact of corrective intervention. Indian Pediatr 2008;45(7):541-6
16. Balachandran R, Vaidyanathan B, Khan A, Kumar RK. Management of undernutrition and failure to thrive in children with congenital heart disease in low-and middle-income countries. Cardiol Young 2017;27(S6):S22-S30.
17. Arodiwe I, Chinawa J, Ujunwa F, Adiele D, Ukoha M, Obidike E. Nutritional status of congenital heart disease (CHD) patients: Burden and determinant of malnutrition at university of Nigeria teaching hospital Ituku – Ozalla, Enugu. Pakistan J Med Sci 2015;31(5):1140-5.
18. Varan B, Tokel K, Yilmaz G. Malnutrition and growth failure in cyanotic and acyanotic congenital heart disease with and without pulmonary hypertension. Arch Dis Child 1999;81(1):49-52.
19. Hassan BA, Albanna EA, Morsy SM, Siam AG, Al Shafie MM, Elsaadany HF, Sherbiny HS, Shehab M, Grollmuss O. Nutritional Status in Children with Un-Operated Congenital Heart Disease: An Egyptian Center Experience. Front Pediatr 2015;15(3):53.
20. National Family Health Survey- 4. Key findings from NFHS-4 fact sheets for key indicators based on final data- Kerala, 2015-16. rchiips.org/NFHS/factsheet_NFHS-4.shtml
Issue: October-December 2018 [Volume 7.4]