Dermatological manifestations in beta thalassemia major patients between 2 to 12 years and their relation with serum ferritine level
Original research
Received:June 1 ,2018; Reviewed: August 7,2018; Accepted:September9 ,2018.
Citation of article: Koushik Roy, Sankar Kumar Das, Avijit Dutta, Rajesh Kumar Mandal , Sankar Kumar Das : Dermatological manifestations in beta thalassemia major patientsbetween 2 to 12 years and their relation with serum ferritine level; New Indian Journal of Pediatric NIJP 2018: 7(3).
Original research
![]()
ABSTRACT
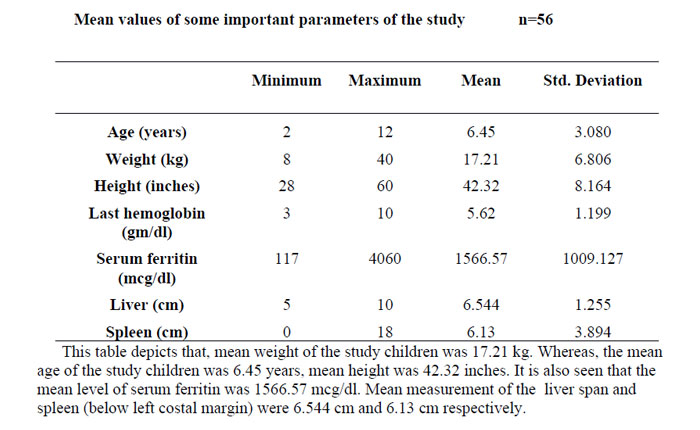
To describe the dermatological manifestations noted in multitransfused beta thalassemia major patients aged between two to twelve years and also to find out any correlation with their serum ferritine level, this study was done. A total 56 thalassemia children were examined for dermatological manifestatios and their serum ferritin levels were measured. Amongst the patients, male to female ratio was 1:1. Most of the study subjects belonged to the Muslim community (64.3%). Dermatological changes were found amongst 94.6% study children and were more frequently seen in females (96.4%). Children belonging to older age group showed increased frequency (100% in >8years) of dermatological changes. Xerosis and Hyperpigmentation were the two most common dermatological changes noted in 66.1% and 53.6% study subjects. Pityriasis versicolor and alba (12.5%), urticaria (5.4%), acanthosis nigricans (8.9%) were other common dermatological manifestation. Besides generalised hyperpigmentation, some subjects (12.1%) were foud to have isolated forehead hyperpigmentation. Less common dermatological changes noted were moluscum contagiosum, diffuse hair loss, nail brittleness, mucosal hyperpigmentation, freckles, acneform eruption, milliaria and pompholyx. The study showed there was a statistically significant correlation between urticaria and the level of serum ferritin(p<0.05). Hyperpigmentation and pityriasis (versicolor & alba) were also more frequent among study groups with higher level of serum ferritin level. However, the statistically significant correlation could not be established due to paucity of data.
INTRODUCTION
Thalassemia is the commonest inherited autosomal recessive single gene disorder seen all over the globe1. Beta-thalassemia results from mutation in the globin gene leading to deficiency, or absence of beta-globin chain synthesis of haemoglobin.
Three percent of world’s population carries alleles for beta-thalassemia2. High prevalence is present in Mediterranean, Middle East, Transcaucasus, central Asia and Indian subcontinent3. In India, among all the hemoglobinopathies, beta-thalassemias are major health problem. Almost 10% of total thalassemic patients worldwideare born in India every year. Overall carrier frequency in India is 3 % to 4%. Certain population in India like Sindhis, Gujratis, Punjabis and Bengalis are more commonly affected with beta thalassemia, incidence varying from 1% to 17%4.
Regular blood transfusion is the main modality of treatment for the correction of anemia of these patients. Repeated blood transfusion along with ineffective erythropoesis and increased iron absorption leads to iron overload in the body.
Several literatures have been published on various systemic complications of beta-thalassemia major, but there is scarcity of literature regarding dermatological manifestations of these patients.
In the current study, we have described different dermatological manifestations noted in multi transfused beta-thalassemia major patients aged between 2 to 12 years attending the thalassemia care unit of North Bengal Medical College. We also tried to establish the correlation between dermatological manifestations with iron overload in the body (measured by serum ferritin level).
MATERIALS AND METHODS
Study type and design: Descriptive observational type with cross sectional design.
Study area: Thalassemia Care Unit and Department of Paediatric Medicine of North Bengal Medical College.
Study period: July 2014 to June 2015.
Study population: Diagnosed cases of beta thalassemia major patients attended to Thalassenia Care Unit or admitted in the Pediatric Ward.
Inclusion criteria: Beta thalassemia major patients between 2 to 12 years age already diagnosed by HPLC or Hb electrophoresis already transfused 10 units of blood.
Exclusion criteria:
- Patients having other systemic diseases with dermatological manifestation.
- Patients aged less than 2 years of age and more than 12 years.
- Patients having pre-existing diagnosed skin disease.
Sample size: All the diagnosed cases of beta thalassemia major patients visited Thalassemia care unit or pediatric outdoor or admitted in the pediatric ward during the study period aged between 2 to 12 years were included in the study keeping the inclusion and exclusion criteria in mind and the sample size ultimately became 56.
Parameters to be studied: Dermatological examination and serum ferritin level.
Plan for data analysis: Datas were entered in Microsoft excel sheet. Then it was analysed by SPSS version 20 software. Datas were further presented by using principles of descriptive statistics that is frequency and percentage. Categorical outcome variables were tested using chi-square test and student test.
RESULTS:
# Others include-moluscum contagiosum, diffuse hair loss, nail brittleness, oral mucosal hyperpigmentation, freckles, acneform eruption, milliaria, pompholyx.
Above table shows that, among all study subjects xerosis was the most common dermatological changes found followed by hyperpigmentation (includes both forehead hyperpigmentation and generalised hyperpigmentation), pityriasis versicolor & alba, acanthosis nigricans, urticaria and others in descending order.
Above table shows that, dermatological changes were present in all children amongst the study group who were having a serum ferririn level more than 1000 mcg/dl and in 83.3% children having less than 1000mcg/dl. This finding is found statistically significant (p<0.05).
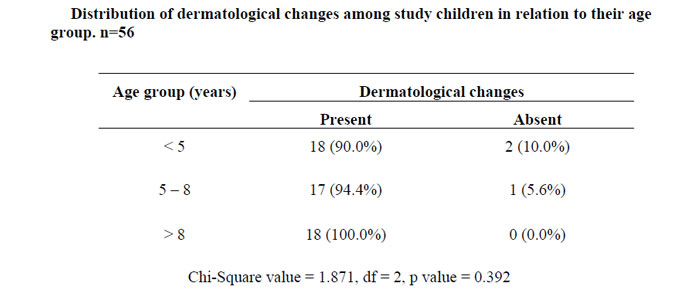
From the above table we came to know that, all the children amongst study who were above the age of 8 years had dermatological changes and amongst the age group of 5 to 8 years and <5years, dermatological changes were found in 90% and 94.4% cases respectively. The findings were found statistically not significant (p > 0.05)
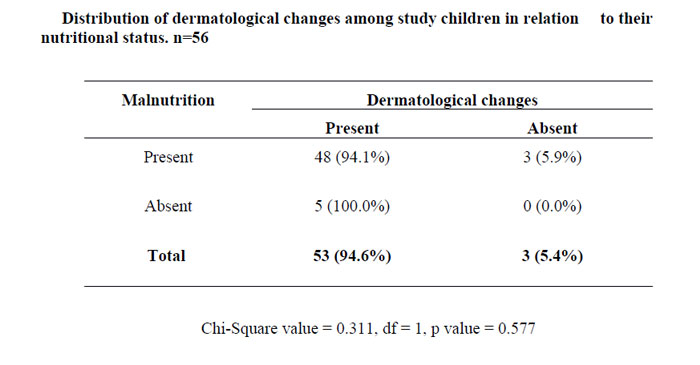
Above table shows that, though most of the children under the study group were malnourished but all of the tiny group of well nourished children were found to have some dermatological changes amongst them(100%) but 94.1% children who were having malnutrition were found to have dermatological changes amongst them. The findings were statistically not significant (p<0.05).
Table no. 2.6 shows that, all children who were having last hemoglobin (Pretransfusion) level more than or equals to 8 gm/dl had dermatological findings and 94.1% of those who were having last 7 gm/dl or less had dermatological changes. The findings were statistically not significant (p>0.05).
Table 2.9 shows that, all those who had spleen size more than or equal to 8cm measured from left costal margin along the splenic axis amongst the study group, had dermatological changes and 95% and 85.7% among those who had 4cm to 7cm and below 4cm spleen size respectively had dermatological changes. The findings was statistically not significant (p>0.05).
Above table shows that, amongst the study children 72.2% whose serum ferritin level were below 1000mcg/dl had Xerosis and those children whose serum ferritin level were between 1000-2000 mcg/dl and more than 2000 mcg/dl, Xerosis was found in 65.2% and 60% respectively. The finding was statistically insignificant (p>0.05).
Above table shows that, Hyperpigmentation were found more commonly in those study children who had serum ferritin level in the higher side i.e. 66.7% who had serum ferritin level more than 2000 mcg/dl, 52.2% who had between 1000 to 2000 and 44.4% who had less than 1000 mcg/dl. The finding was not statistically significant (p>0.05).
Above table shows that Pityriasis were found more (20%) amongst the study children who had Serum Ferritin level more than 2000 mcg/dl than who had Serum Ferritin between 1000 to 2000 (13%) and who had less than 1000 mcg/dl. The finding was statistically not significant (p>0.05).
Above table shows that, Acanthosis nigricans were not present amongst the study children who had serum ferritin level <1000 mcg/dl, present amongst 17.4% who had between 1000 to 2000 and amongst 6.7% who had more than 2000 mcg/dl. The finding was statistically insignificant (p>0.05).
Above table shows that Urticaria was only present amongst the study children who had a serum ferritin level more than 2000 mcg/dl and the finding was statistically significant (p<0.05).
DISCUSSION:
Amongst the total 56 patients, male to female ratio was 1:1. Most of the study subjects belonged to the Muslim community(64.3%). Dermatological changes were found amongst 94.6% study children and were more frequently seen in females(96.4%).Children belonging to older age group showed increased frequency(100% in >8years) of dermatological changes.
Similar related study by Al-Rubiay KK et al. conducted among 195 thalassemia patients in Iraq, noted dermatological changes among all subjects5. Another study done by Dogramaci A.C. et al. in Turkey, among 78 thalassemic children dermatological changes were noted in 83.3% study subjects, and males showed much higher frequency (64.1%) than females(35.9%)9.
In the present study, subjects having pre-transfusion haemoglobin level ≥8gm/dl had increased frequency of dermatological changes. Dermatological changes were also more common among study groups with more hepatic span (≥7cm liver span), as well as with large spleen size (≥8cm measured from left costal margin along splenic axis) .
No relationship was found between nutritional status of the study subjects with dermatological change.
In the present study, xerosis was the most common (66.1%) dermatological change amongst the study subjects, followed by skin hyperpigmentation(53.6%). skin hyperpigmentation was noted as generalised hyperpigmentation(87.1%) as well as only forehead hyperpigmentation (12.9%).
Xerosis, the most common(64.1%) dermatological change among thalassemia major patients by Al-Rubiay KK et al. in Iraq, was comparable to our study5.Bronzy coloured skin(54.9%) was the second most common dermatological change noted in their study, but similar skin changes was not found in the present study subjects. Another study by Momeni A et al. also showed xerosis as the most common(53%) dermatological change manifested among beta-thalassemia major subjects in Iran7.Dogramaci A.C. et al. noted xerosis in 34.6% study subjects in Turkey9. The cause of xerosis may be due to excess iron storage in the body.10
Hyperpigmentation was found in 48.7% study subjects in the study done by Al-Rubiay KK et al. in Iraq5. Momeni A et al. noticed hyperpigmentation at the injection site of desferral administration among 30% study subjects7. Idiopathis Guttate Hypermelanosis was noticed amongst 6.4% subjects in the study done by Dogramaci AC et al9. The cause of hyperpigmentation may be due to cutaneous Iron deposition which subsequently damages the skin and also enhances melanin production11.
In the current study, generalised hyperpigmentation was more frequent (n= 27, 48.2%) as compared to most of the other studies. Higher incidence is probably due to irregular chelation therapy and higher iron overloaded state in our study subjects. Moreover, isolated hyperpigmentation on forehead was noted among four study subjects (7.1%) and such finding was not noted in any other earlier studies as per literature search in English language with the best of efforts. Cause of this isolated hyperpigmentation could not be explained.
Acanthosis nigricans was also found in 8.9% patients, pityriasis versicolor and alba, accounted for 12.5% of all the skin changes seen. Urticaria was another important skin change noted in 5.4% study children.
Other less common dermatological changes included moluscum contagiosum, diffuse hair loss, nail brittleness, oral mucosal hyperpigmentation, freckles, acneform eruption, milliaria, pompholyx. The incidence of these skin changes comprised of 17.9% among total study subjects.
However, Naderi M. et al. in 2013, reported freckles(70.7%) as the most common dermatological finding amongst their patients with beta-thalassemia major, in Iran6. Another study by Dogramaci A.C et al reported pruritus(37.2%) as the most common dermatological changes followed by xerosis(34.6%) and scarring(24.4%) in their study subjects in Turkey9.
The present study was aimed at elucidating the correlation between serum ferritin and skin manifestations in the patients suffering from beta thalassemia major, and to see if at all, a high serum ferritin level may preclude a skin manifestation or vice-versa.
Aessopos A. et al, found 26% of the study subjects had either angioid streaks or pseudoxanthoma elasticum skin lesions or both8. However, no relation was found between these skin lesions withserum ferritin levels. Dogramaci A.C et al. found higher mean serum ferritin level among patients with xerosis9.
In the present study, xerosis was the most common dermatological manifestation, but no relation between xerosis and serum ferritin level was found. Hyperpigmentation (generalised and isolated forehead), was the second most common dermatological change found in the present study and was directly proportional with serum ferritin levels. However, this finding was statistically not significant (p>0.05).
Urticaria was seen in 5.4% of study children. Moreover, urticaria was found only in those patient who had serum ferritin level more than 2000 mcg/dl and the correlation was found to be statistically significant (p<0.05). Dogramaci A.C et al also found urticaria among 3.8% study population9.
The average incidence of urticaria among Indian children is around 2.5%12. The higher incidence of urticaria among our study groups may be due the allergic reaction in response to plasma proteins following repeated blood transfusion13.
Pityriasis versicolor and pityriasis alba was also found to be directly proportional with serum ferritin level, but the correlation was statistically insignificant (p>0.05).
Acanthosis Nigricans was found in 8.9% of study subjects, and not correlated to the serum ferritin level.
CONCLUSION:
- Beta-thalassemia major is equally distributed amongst male and female subjects in the present study.
- Most of the patients belonged to the Muslim community.
- Dermatological manifestations were seen more among older multi-transfused betathalassemic children.
- Dermatological manifestations were more commonly seen in females.
- Common dermatlogical changes noted in our study were xerosis (66.1%), hyperpigmentation (53.6%), pityriasis versicolor & alba (12.5%), acanthosis nigricans (8.9%), urticaria (5.4%). Other less common finding were moluscum contagiosum, diffuse hair loss, nail brittleness, mucosal hyperpigmentation, freckles, acneform eruption, milliaria, and pompholyx.
- Xerosis was the most common dermatological change noted in the study followed by Hyperpigmentation.
- A definite relationship between Dermatological change with serum ferritin level was noted in the present study,though it was statistically not significant.
- Relation between serum ferritin level and Urticaria was statistically significant.
- A relationship also found between hyperpigmentation and Pityriasis with serum ferritin level, but it was statistically insignificant. Furthur study with larger sample size is needed.
BIBLIOGRAPHY:
1. WHO. Genes and Human Disease. Genomic Resource Centre. 2015 (http://www.who.int/genomics/public/geneticdiseases/en/).
2. Kliegman, Stanton, St Geme, Schor. Nelson Textbook Of Pediatrics. 20th ed. 2015; 2349- 2353.
3. Weatherall DJ, Clegg JB: The Thalassemia Syndromes. Oxford: Blackwell Scientific Publications 2001.
4. Kirti Grow, Minakshi Vashist, Pankaj Abrol, Shiksha Sharma, Ritu Yadav: Beta Thalassemia In India: Current Status And The Challenges Ahead. Int J Pharm Pharm Sci, Vol 6, Issue 4; 28-33.
5. Kathem K, Al-Rubiay, Omran S, Habib and Samira M Ebrahim: The Pattern of skin diseases in Basrah Province: Review of 9252 patients.MJBU 1995,13:183-190.
6. Majid Naderi , Hami Shamshiri , Shaban Alizadeh , Akbar Dorgalaleh , Rima Manafi, Shadi Tabibian: Cutaneous and mucosal manifestations in patients with beta major thalassemia: Dermatology and Cosmetic 2013; 4(1): 27-33.
7. Momeni A, Adabi M, Amin Javaheri M, Hoorfar H: Skin and mucosal manifestations in patients with thalassemia major: Journal of Babol University of Medical Science (JBUMS) 2001; 3(2(10)):38-46.
8. Athanasios Aessopos, Panayotis Savvides, George Stamatelos, Thomas Tassiopoulos, Phaedon Kaklamanis, Phaedon Fessas, Loannis Rombos, Markisia Karagiorga: Pseudoxanthoma elasticumlike Skin Lesions and Angioid Streaks in beta- Thalassemia:American Journal of Hematology 41; 159-164 (1992).
9. Asena Cigdem Dogramaci, Nazan Savas, Burcin Ozer and Nizami Duran : Skin diseases in patients with beta-thalassemia major: International Journal of Dermatology 2009; 48, 1057–1061.
10. Jeffrey K. Aronson, Leopold Meyler, Maurice Nelson Graham Dukes: Meyler’s Side Effect Of Drugs, Annual 34. 2012; 367.
11. Deborah Round and Eliezer Rachmilewitz : New England Journal of Medicine 2005; 353(11):1135-46.
12. Kaliaperumal Karthikeyan, Devinder Mohan Thappa and B.Jeevankumar: Pattern of Pediatric Dermatoses in a Referral Center in South India. Indian Pediatrics 2004; 41:373-377.
13. Renzo Galanello, Raffaella Origa : Management of Thalassaemia; IRON2009_CAP.11(264-285):EBMT2008 4-12-2009.
Issue: July-September 2018 [Volume 7.3]