Clinico-Epidemiological Profile And Patterns Of Antibiotic Sensitivity Of Enteric Fever Cases Among Paediatric Patients In The Adjacent areas of Midnapore – A hospital-based study
Original research
Address of the institution where the work was carried out: Department of paediatrics and department of Microbiology, Midnapore Medical College & Hospital, West Midnapore, West Bengal, India.
Corresponding author: Dr. Souvik Biswas, department of Paediatrics, Midnapore Medical College & Hospital, West Midnapore, West Bengal, India. Email ID: dr.souvikbiswas.ped@gmail.com
Received: June 12 ,2017; Reviewed: July 27,2017; Accepted:September 9 ,2017.
Citation of article: Tarapada Ghosh*, Souvik Biswas**Ranjita Santra (Dhali)***, Partha Sarathi Satpathi : Clinico-Epidemiological Profile And Patterns Of Antibiotic Sensitivity Of Enteric Fever Cases Among Paediatric Patients In The Adjacent areas of Midnapore – A hospital-based study ; New Indian Journal of Pediatric NIJP 2018: 7(3)
Original Research
![]()
Abstract
Aims: The disease burden of enteric fever has increased due to overwhelming resistance of Salmonella. The objectives of this study were to assess different clinico-epidemiological factors and biochemical profiles of blood-culture positive cases as well as to detect the antibiogram for its treatment.
Materials & Methods: Based on inclusion and exclusion criteria, 50 children of age 1-12 years out of 239 screened were culture positive and constituted the study group. Across-sectional observational study was conducted for a period of one year. A detailed clinical examination, blood culture and antibiogram were performed. The total duration of treatment with antibiotics was two weeks. The clinical course was monitored and the period of defervescence noted in the study subjects.
Results: School-going children (56%) were mainly affected though incidence is increasing in under-5 age group (24%). The pattern of fever was predominantly continuous (48%) and high grade. Prior exposure to antibiotics was statistically significantly (p=0.03) in the cases < 5 years. S. typhi was 92% and 89.5% sensitive to Azithromycin and Cefixime while in S. paratyphi the sensitivity was 91.7% and 100% respectively. Occurrence of S. paratyphi Ainfection and early defervescence was statistically significant (p=0.03).
Conclusion: Lower socioeconomic status was responsible for higher incidence rate. Widal test with moderate sensitivity and specificity is still a useful diagnostic tool. It was re-established that Ceftriaxone, Cefixime and Azithromycin were the most effective anti-salmonella agents.Re-emergence of chloramphenicol susceptibility and resistance to ciprofloxacin was observed, thereby emphasizing rational drug use in enteric fever.
Keywords: enteric fever, anti-salmonella agents, antibiogram, Kirby-Bauer Disc Diffusion technique, Widal test
Introduction: Enteric fever is a global public health problem with an annual incidence of at least 26.9 million cases reported worldwide of which 1% result in death. [1]Majority of the cases are seen in Asia and sub-Saharan region of Africa. In India the disease is endemic with morbidity ranging from 102 to 2219 per 100000populations. [2]Due to the lack of microbiological facilities in developing countries, theseestimates may be more representative of the clinical syndrome rather than of culture-provendisease. If not treated properly enteric fever has 30% mortality which reduces to as low as 0.5% through appropriate treatment.[3]Caused by Salmonella typhi and Salmonella paratyphi, Enteric fever is one of the common causes of fever in children with variedpresentation and significant difference in the signs and symptoms compared to adults. The disease burden is compounded by explosive emergence ofmultidrug resistant salmonellae which are resistant to conventionally used drugs likechloramphenicol, ampicillin and cotrimoxazole. The fluoroquinolones, other second-lineantibiotics, such as third-generation cephalosporins (e.g. ceftriaxone and cefixime), andazithromycin are currently regarded as the antibiotics of choice for treating MDR strains. However, an issue of great concern is the emergence of strains of S. Typhi and S. Paratyphiwith reduced susceptibility to fluoroquinolones. Furthermore etiological diagnosis like blood culture which is the gold standard of the diagnosis is available in relatively few centers. In this backdrop this study was conducted with the objective to know the clinico-epidemiological as well as biochemical profile of enteric fever cases and its antibiogram in and adjacent areas of Midnapore.
Materials and Methods A cross-sectional observational single centre study with 50 culture-positive enteric fever cases was conducted from May 2014 to April 2015. Patients aged between 1 – 12 years of both sexes with fever of ≥3 days admitted in paediatric ward of Midnapore Medical College & Hospital were eligible. Informed consent was taken from the parents of the study sample and purpose of study was explained in local language (Bengali) or English. Ethical clearance was obtained from Institutional ethics committee (IEC) of Midnapore Medical College & Hospital, West Midnapore. A detailed clinical history, thorough clinical examination and laboratory investigations & appropriate treatment at the time of admission and during course of hospital stay was performed in all cases and findings were recorded in a pre-designed proforma. For blood culture, blood was collected in Bile broth and incubated in room temperature. When bottles showed signs of positive growth, they were cultured on Blood agar on day 3 and 7. Salmonella spp. isolates were identified with specific anti-sera and standard biochemical tests. Kirby-Bauer Disc Diffusion technique was used to analyze drug sensitivity pattern. The pattern of antibiotic sensitivity specially if there is any indication of multidrug resistance was noted. The patients with a presumptive clinical diagnosis of enteric fever were treated with parenteral ceftriaxone. The clinical course was monitored and the period of defervescence recorded. Total duration of treatment with antibiotics was 14 days.
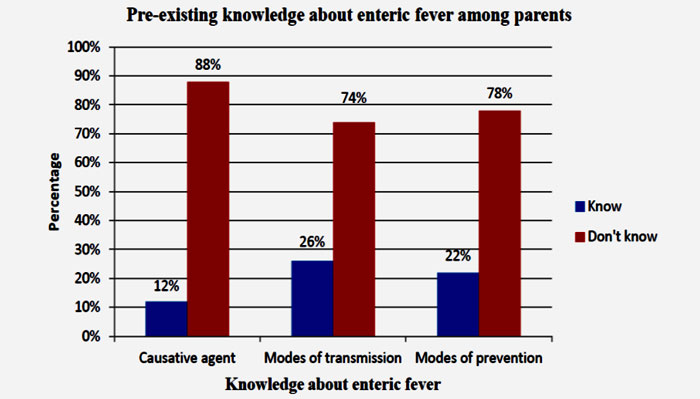
Results: Based on inclusion and exclusion criteria, a total of 239 children were screened for enteric fever. Out of them, 50 children were found to be culture positive and they formed the study group. In the present study the incidence of typhoid fever as found in the children of age group 5-10 years was 56% and that of under-5 children were 24% as shown in figure 1. Among the study subjects, boys were 62% and girls constituted remaining 38%.In our study, most of the cases occurred in monsoon (46%) season followed by pre-monsoon (32%) period as shown in figure 2. It was detected that 46% were from the rural area and38% from urban slum. About 44% of children were in per capitaincome group 500-999, majority of the subjects (44%) resided in kachcha house, 30%of the parents had a primary level education and 40% were illiterate. Majority of the population (90%) did not take any measure to treat water before drinking; only 8% of them used chlorination as a method of water treatment followed by boiling (2%) as evident from figure 3. Majority (66%) of the affected children were taught to practice open-air defecation and only 12% cases practiced proper hand washing techniques before consuming meals. Only 12% parents knew about the causative agent as bacteria though they could not name the organism, 26% knew about modes of transmission of the disease while merely 22% of them knew about modes of prevention of the disease as shown in figure 4. Most of the children (38%) had a history of fever for 5 – 7 days while 14% of them had history of fever >14 days. Majority of the subjects got admitted with high grade fever of which 34% had temperature 102.1 – 103 °F while 6% had temperature >104 °F, and only 8% had low grade fever. About 48% of the cases had history of continuous fever while 44% had remittent fever as evident from table 1. It was detected that 34 patients did not take any form of antibiotics prior to admission. Other than fever which was present in all cases, anorexia (84%), headache or myalgia (38%), nausea & vomiting (36%), cough (34%) diarrhoea (28%) and pain abdomen (24%) were the predominant symptoms as shown in table 2. Complications like altered sensorium and GI bleeding occurred in 10% and 4% cases respectively. Hepatomegaly and splenomegaly were present in 46% and 28% of cases as shown in table 3. Laboratory investigation revealed that 74% of the patients had Hb value <11 gm%. 20% of the cases had leukocytosis and 14% had leukopenia. Eosinopenia occurred in 14% cases. SGOT and SGPT levels were elevated in 24% and 32% of cases respectively . To titre≥ 1:160 was found in 84% of the subjects while TH titre≥ 1:160 was observed in 78%. Salmonella typhi constituted 76% of the isolated organism while Salmonella paratyphi A constituted remaining 24%. In our study S. typhi was 100% sensitive to Ceftriaxone. It was around 92% and 89.5% sensitive to Azithromycin and Cefixime respectively as shown in as shown in figure 5. Resistance to Ciprofloxacin and Nalidixic acid was around 34% and 71% respectively. Resistance to 1st line drugs like Ampicillin, Cotrimoxazole and Chloramphenicol were 79%, 84% and 31.6% respectively. In our study S. paratyphi was 100% sensitive to Ceftriaxone and Cefixime while azithromycin was 91.7% sensitive as shown in the figure 6. Resistance to Ciprofloxacin and Nalidixic acid were around 33.3% and 66.7% respectively. Resistance to 1st line drugs like Ampicillin, Cotrimoxazole and Chloramphenicol found were 75%, 83.3% and 33.3% respectively. There was statistically significant early response to Salmonella paratyphiA treatment indicating that it was a milder form of enteric fever. Association between prior antibiotic use and age was found to be significant which indicates that prior antibiotics were given more in case of under-5 children than ≥5 year age group.
Discussion: In our study maximum incidence of enteric fever was seen in children in the age group of 5 – <10 years (56%), followed by those under 5 years of age accounting for 24% cases. Similar results have been reported in studies by Vollaard AM, et al[4] in Indonesia, R K Arora in Kolkata[5] and A Sharma in Rohtak[6]. However, few studies, like the ones conducted by A. Sinha, et al in Delhi[7] and S.K. Saha, et al in Bangladesh[8] have reported higher incidences of enteric fever in the under 5 age group (44% and 54% respectively). In our study, boyswere predominantly affected by enteric fever, contributing to 62% of the cases Similar male preponderance have been reported in studies conducted by Raghuraman TS et al in Bangalore[9] and Malla T, et al in Nepal[10] (66% and 60% male preponderance respectively). This might be attributable to our cultural background. In our patriarchal society, males engage more in outdoor activities, thereby contracting infections and with a higher likelihood of reporting to hospitals. Majority of our study subjects belonged to the lower socioeconomic status and approximately 40% parents of the patients were illiterate. Similarresults were observed in studies by Srikantiah P, et al done in Uzbekistan [11] and Kumar R et al in Delhi[12]. Knowledge about modes of transmission and prevention of enteric fever among the parents was very poor. A low socioeconomic status is reflective of poor standards of living, ignorance, illiteracy and poor personal hygiene, increasing the susceptibility to infections like enteric fever. It was observed that majority (66%) of the affected children were taught to practice open-air defecation, thereby emphasizing the protective effects of sanitary latrine use from enteric fever. This view has been supported by different other studies conducted previously in Dhaka, Jakarta and Darjeeling.[13,14,15] In the present study, 90% of the subjects had no access to safe drinking water and only 12% cases practiced proper hand washing techniques before consuming meals. The aforesaid data are in accordance with the above mentioned three studies thereby establishing a significant association between use of unsafe water, unhealthy practices and a lack of personal hygiene with the development of enteric fever. In our study, most of the cases (46%) occurred during monsoon season followed by 32% cases in the pre-monsoon period. Similar observations were made in two studies conducted by Mohanty S et aland Dewan AM et alin Delhi and Bangladesh respectively.[16, 17] The above data indicate that maximum disease transmission occur during summer and rainy seasons. Fever was the main presenting symptom in all the cases which is in conformity with different other studies.[2,12,18,19] Fever lasted for five days or more in majority of cases (82%) at presentation. The pattern of fever was predominantly continuous (48%) and high grade. Vomiting, anal pain and diarrhoea were seen in 36%, 24% and 28% patients respectively in accordance with the studies by Jog S et al[19] and Ganesh R et al[20] respectively. In the present study, 34% cases complained of cough as an associated symptom, similar to the finding of ther studies.[6,12] GIT bleeding was observed in two cases, similar to the findings by Sharma et al[6] but was contradictory to the findings by Kumar R et al.[12] Coated tongue was present in 44% of the cases, similar to a recent study.[20] In this study isolated hepatomegaly was observed in 46% cases, while 28% patients presented with isolated splenomegaly which is similar to the findings of a study[6] and in discordance with the results of previous two studies[12,20] both of which reported a much higher incidence of organomegaly. 66% of our patients were found to have normal leukocyte counts (4000 – 11000), 14% had leukopenia and 20% showed leukocytosis. The results were in agreement with Gavhane J et al and Jog S et al both of which were conducted in Mumbai.[18,19] Eosinopenia was seen in seven children (14%), while absolute eosinopenia was noted in only two cases. The data is supported by Gavhane J et al[18] but in contrast to the findings by Jog S et[19] and Ganesh R et al[20] which reported absolute eosinopenia in 77% and 72% cases respectively. Anaemia was present among 74% of the children, which is higher than previous report.[12] The possible explanation lies in the fact that nutritional iron-deficiency anaemia is widely prevalent in our study population. Serum SGPT and SGOT were elevated in 32% and 24% cases respectively, consistent with previous observations.[18,19] TO and TH titres remained elevated (≥ 1:160 ) in 84% and 78% cases respectively, indicating that Widal test is still a useful, cheap and easily accessible tool for diagnosis of enteric fever. Among 239 suspected cases of enteric fever, 50 cases (21%) were culture-positive, in conformity with studies by Chowta MN et al and Malla T et al.[2,10] In our study 16 children (32%) had received some antibiotic treatment for a period of 1 – 4 days before blood culture was done. Despite this they were still found to be culture-positive on evaluation. Prior use of antibiotics leading to poor yield on culture is often cited as a reason dissuading clinicians from sending blood cultures in a patient with fever without focus. However results of our study advocate that blood cultures should be sent in suspected enteric fever cases even if the patient has received prior antibiotics. Gavhane J et al and Jog S et al also reported similar results in their studies.[18,19] A significant majority (76%) of the culture-positive enteric fever cases were due to S. typhi while only 24% cases were caused by S. Paratyphi A. The data are in accordance with the studies conducted by Mohanty S et al[16] in Delhi and Krishnan P et al[21] in Chennai which showed S.Typhi as main causative organism in 76% and 70% of cases respectively. On the contrary, studies conducted in New Delhi, Nagpurand Chandigarh showed a significantly higher isolation rates of S. Paratyphi A estimated at 44.9%, 46.1% and 40.6% respectively.[22,23,24] In the present study a high prevalence of nalidixic acid resistance (approximately 70%) was noted which was in conformity with recent reports.[16,21,24] Nalidixic acid resistant Salmonella isolates are endemic in the Indian subcontinent. An unpredictable response to treatment with ciprofloxacin has been observed in patients infected with such strains. This resistance is however not detected by disc diffusion method using the recommended breakpoints in diagnostic laboratories, resulting in ciprofloxacin being administered as the drug of choice to treat typhoid fever. This may delay the decision to switch over to third generation cephalosporins or other appropriate antibiotics. Re-emergence of chloramphenicol susceptibility was observed in our study. Susceptibility of S. Typhi and S. Paratyphi to chloramphenicol were 68.4% and 66.7% respectively. Studies undertaken by Dutta S et al[25] in Kolkata and Mohanty S et al[16] in NewDelhi reported similar observations indicating a changing pattern ofchloramphenicol susceptibility. Though a study conducted by Saha SK et al[8] in Bangladesh reported ceftriaxone-resistant salmonella strains, this study revealed that all isolated salmonella strains were fully sensitive to ceftriaxone, consistent with different recent studies.[2,16,21,24] S. typhi was around 92% and 89.5% sensitive to Azithromycin and Cefixime respectively while in cases of S. paratyphi the sensitivity was 91.7% and 100% respectively. Significant association (p=0.03) was observed between S. Paratyphi A infection and early defervescence indicating that it was a milder form of enteric fever. The present study also showed that prior antibiotic use was significantly higher (p=0.03) in under 5 age group that might be due to a greater concern of parents seeking medical help at the earliest for their children.
Conclusion: In the present study the subjects who belong to the lower socioeconomic status were mainly affected. Drinking unsafe water, not having a sanitary latrine at home, and poor hand washing practices were found to be the primary epidemiological risk factors of enteric fever. We found detected that although Widal test has moderate sensitivity and specificity, it is still a useful, cheap and easily accessible tool for diagnosis of enteric fever. Our study advocates that blood cultures should be sent in suspected enteric fever cases even if the patient has received prior antibiotics. Cephalosporins mainly ceftriaxone followed by cefixime were the most effective antimicrobials for the treatment of enteric fever followed by the macrolide antibiotic azithromycin. Hence, considering the increase in resistance to ciprofloxacin and re-emergence of sensitivity to chloramphenicol, the policy of treatment of enteric fever needs to be rationalized.
Contributtion of authors: TG and PSS conceptualized the study plan and developed the strategy for work; SB did the data collection, statistical analysis and drafted the manuscript; RSD aided in preparation of the manuscript and revised it critically with her intellectual inputs.
Conflict of Interest: None
Funding: Nil
Learning points: What is already known on this topic?
1. The vast majority of enteric fever disease burden is witnessed in Asia.
2. Given the paucity of microbiological facilities in developing countries, the figures relating to endemicity with morbidity as well as mortality are representative of the clinical syndrome rather than of culture-proven disease.
3. The increase in enteric fever cases could possibly be due to high degree of clinical suspicion with mild fever cases being investigated for enteric fever, changing host susceptibility, change in virulence of the organism and widespread use of fluroquinolone.
What this paper adds?
1. Widal test in India continues to be important in the investigation of patient with fever despite its variable sensitivity and specificity in the era of multidrug resistance.
2. Significant percentage of culture sensitivity even after use of antibiotics has been detected specially to cephalosporins and macrolides i.e. azithromycin. So an attempt should be made to send blood culture
3. Considering the increase in resistance to ciprofloxacin and re-emergence of sensitivity to chloramphenicol, the policy of treatment needs to be rationalized.
References
1. Kliegman RM, Stanton BF, Geme JWS, Schor NF, Behrman RE. Nelson Textbook of Pediatrics, 20th ed., Philadelphia: Elsevier Saunders 2016; 1388-93
2. Chowta MN, Chowta NK. Study of Clinical Profile and Antibiotic Response in Typhoid Fever. Indian J Med Microbiol 2005; 23(2): 125-27.
3. Cooke FJ, Wain J. The emergence of antibiotic resistance in typhoid fever. Travel Med Infect Dis 2004; 2: 67-74.
4. Vollaard AM, et al. Risk Factors for Typhoid and Paratyphoid Fever in Jakarta, Indonesia. JAMA 2004; 291(21): 2607-15
5. Arora RK, Gupta A, Joshi NM, et al. Multidrug resistant typhoid fever. Study of an outbreak in Calcutta. Indian Pediatr 1992; 29:61-66
6. Sharma A, Gathwala G. Clinical profile and outcome of enteric fever. Indian Pediatr 1993; 30 (1): 47-50.
7. Sinha A, Sazawal S, Kumar R, Sood S, Reddaiah VP, Singh B, Rao M, Naficy A, Clemens J, Bhan MK. Typhoid fever in children aged less than 5 years. Lancet 1999; 354:734-737.
8. Saha SK, Baqui AH, Hanif M, Darmstadt GL, Ruhulamin M, Nagatake T, Santosham M, Black R. Typhoid fever in Bangladesh: implications for vaccination policy. The Pediatric Infectious Disease Journal 2001; 20: 521-4.
9. Raghuraman TS, et al. Clinical Profile and Therapy in Enteric Fever. Indian Pediatr 1994; 31 (2): 196-99.
10. Malla T, et al. Enteric Fever: A retrospective 6-year analysis of 82 paediatric cases in a teaching hospital. Kathmandu University Medical Journal 2007; 5: 181-87.
11. Srikantiah P, et al. Epidemiology and risk factors for endemic typhoid fever in Uzbekistan. Tropical Medicine and International Health 2007; 12: 838-47.
12. Kumar R, Gupta N, Shalini. Multidrug-resistant Typhoid fever. Indian Journal of Pediatrics 2007; 74(1): 39-42.
13. Ram PK, Naheed A, Brooks WA, Hossain MA, Mintz ED, Breiman RF. Risk factors fortyphoid fever in a slum in Dhaka, Bangladesh. Epidemiol Infect 2007; 135(3):458-65.
14. Vollaard AM, et al. Risk Factors for Typhoid and Paratyphoid Fever in Jakarta, Indonesia. JAMA 2004; 291(21): 2607-15.
15. Sharma PK, Ramkrishnan R, Hutin Y, Manickam P, Gupte MD. Risk factors for typhoid in Darjeeling, West Bengal, India: evidence for practical action. Tropical Medicine and International Health 2009; 14(6): 696-702.
16. Mohanty S, Renuka K, Sood S, Das BK, Kapil A. Antibiogram pattern and seasonality of Salmonella serotypes in a North Indian tertiary care hospital. Epidemiol Infect 2006; 134, 961–66.
17. Dewan AM, Corner R, Hashizume M, Ongee ET. Typhoid Fever and Its Association with Environmental Factors in the Dhaka Metropolitan Area of Bangladesh: A Spatial and Time-Series Approach. PLOS Neglected Tropical Diseases 2013; 7(1): e1998.
18. Gavhane J, Yewale V, Weekey P, Dhanya, Warrior D. Enteric Fever in children from Navi Mumbai – clinical Profile, hematological features, sensitivity patterns and response to antimicrobials. Pediatric Infectious Disease 2010; 2(1):5-9.
19. Jog S, Soman R, Singhal T, Rodrigues C, Mehta A, Dastur FD. Enteric Fever in Mumbai – Clinical Profile, Sensitivity Patterns and Response to Antimicrobials. JAPI 2008;56: 237-40.
20. Ganesh R et al. Profile of Typhoid Fever in Children from a Tertiary Care Hospital inChennai-South India. Indian Journal of Pediatrics 2010; 77: 1089-92.
21. Krishnan P, Stalin M, Balasubramanian S. Changing trends in antimicrobial resistance of Salmonella enterica serovar Typhi and Salmonella enterica serovar paratyphi A in Chennai. Indian Journal of Pathology and Microbiology 2009; 52(4): 505-8.
22. Sood S, Kapil A, Dash N, Das BK, Goel V, Seth P. Paratyphoid fever in India: an emerging problem. Emerging Infectious Disease 1999; 5: 483-84.
23. Tankhiwale SS, Agrawal G, Jalgaonkar SV. An unusually high occurrence of Salmonella enterica serotype Paratyphi A in patients with enteric fever. Indian J Med Res 2003; 117: 10-2.
24. Gupta V, Kaur J, Chander J. An increase in enteric fever cases due to Salmonella Paratyphi A in & around Chandigarh. Indian J Med Res 2009; 129: 95-98.
25. Dutta S, Sur D, Manna B, Bhattacharya SK, Deen JL, Clemens JD. Rollback of Salmonella enterica serotype Typhi resistance to chloramphenicol and other antimicrobials in Kolkata, India. Antimicrob Agents Chemother 2005; 49:1662-3.
Figure 1: Age distribution of cases
Figure 2: Distribution of cases according to the seasonal variation
Figure 3: Distribution of cases according to treatment of drinking water
Figure 4: Pre-existing knowledge about enteric fever among the parents
Figure 5: Antibiotic sensitivity pattern of S typhi
Figure 6: Antibiotic sensitivity pattern of S paratyphi
Table 1: Distribution of cases according to the type of fever at admission (n=50)
Table 2: Distribution of cases according to the clinical symptoms (n=50)
Table 3: Distribution of cases according to the clinical signs (n=50)
Issue: July-September 2018 [Volume 7.3]