Cough Profile and Trends in Cough Management in Children across India: Results of a Multi-centric, Cross-sectional Survey
ORIGINAL RESEARCH
Corresponding author: Dr. Nimain Mohanty, Professor, Department of Pediatrics, MGM Medical College, Navi Mumbai
ABSTRACT:
Objective: To find the nature of cough associated symptoms and conditions, medication preference in Indian children visiting pediatric outpatient services, with cough as the chief complaint.
Material and methods: The survey was conducted in six cities across Indian winter months from October to December 2017. The target population for the survey consisted of 1998 children, involving200 pediatricians across the country. Data was collected on children having cough, categorized under 6 groups ranging from age 1-2 years to 11-12 years, visiting pediatric OPD / clinics with cough as the chief complaint. Parameters evaluated included duration of presenting cough, history of similar episodes, nature, intensity and frequency of cough, associated symptoms, presence of risk factors, drugs used for treatment of cough, concomitant medications and self-medication, if any.
Results: Data on 1998 children having cough, aged between 1 to 12 years (58% males; 42% females), wascapturedin this survey in 6 cities(Bangalore – 350, Ahmedabad – 249, Delhi – 403, Hyderabad – 298, Lucknow – 397 and Mumbai–301). Over69% children presented with cough since5 days prior to OPD visit while only 3% had symptoms lasting over 10 days. Almost half of the children reported 4 to 6 similar episodes of cough in preceding 12 months. 25% of the children were having dry cough whereas 61% had wet cough with no or scanty expectoration. Fever was present as associated symptom in 62.9% cases. Majority (77%) of children had no family history of asthma, allergic rhinitis or tuberculosis. None of them were diagnosed either as pneumonia or tuberculosis on further investigation. First and second generation antihistaminics were prescribed in 76% and 78% children respectively. Antibiotics (50%) and nutritional supplements (12%) were also prescribed besides mucolytics (62%) and expectorants (63%). 83% of children preferred oral medicine. More than half of the children had more than 6 bouts of cough per day. Use of self-medication was however low.
Conclusion: Acute onset and recurrent cough is common in children. Exposures to modifiable risk factors such as environmental pollutants are commonly seen to be associated with pediatric cough. Fever is a common accompanying symptom. Due caution need be observed while prescribing multiple and multi-combination preparations so that same molecule is not present in different preparations, thus avoiding overdosing. Decongestants, antitussives, mucolytics, expectorants and first and second generation antihistamines were commonly prescribed in management of pediatric cough with a view to decrease mucosal oedema, secretions and allergy.
Key words: Cough, children, survey, symptoms
Introduction: Cough is an important natural defence mechanism of respiratory tract. It could also be a warning sign of several respiratory and non-respiratory diseases and is one of the most common reasons for both adults and children seeking medical aid. Acute or short-lived cough often occurs in association with upper respiratory tract infection, is usually of viral etiology, self-limiting and mostly resolves within three weeks13. Almost 30% of them have associated multi-trigger wheezing.
Under diagnosis of asthma re-emphasized cough as a symptom being taken seriously. On the other hand, there is increasing evidence that children are inappropriately treated for asthma, based on cough as the sole symptom14,23. Coughing in children can be distressing and can have a major impact on child’s sleep, school performance and ability to play. It may similarly disturb other family members’ sleep and be disruptive for school teachers. Considerable parental anxiety is generated in families with a child with problem of coughing4,9.
Cough is the most common pediatric problem managed by family physicians (FP), and it is more common in preschool children than older children. Most cough in children are caused by undifferentiated acute respiratory tract infections—a cough that does not conform to any clear diagnostic syndrome such as croup, whooping cough, pneumonia, or bronchiolitis24. Causes of cough include acute respiratory tract infection, asthma, non-asthmatic eosinophilic bronchitis, exposure to environmental irritants such as – smoke, dust, gastroesophageal reflux, rhinitis, sinusitis, post-nasal drip, laryngopharyngeal reflux, obstructive sleep apnea or drug induced cough. Cough management is based on the cause, type of cough, duration and severity. Symptomatic treatment options for cough include antitussives, mucolytic agents, expectorants and bronchodilators, whereas definitive treatment depends on the underlying cause. Despite the high prevalence of cough in children, the topic has been poorly researched9.
Narayanan et al (16) had conducted a detailed profiling survey in India in patients visiting family physicians with cough as the chief complaint. However, the study involved of a very limited population from pediatric age group. Hence this survey of similar kind was undertaken to understand and generate data on nature of cough, associated symptoms/conditions and the medication preference in Indian children visiting pediatric outpatient departments (OPD) with cough as the major complaint.
Material and methods
This cross sectional questionnaire based survey was conducted among children aged 1 to 12 years,visiting pediatric OPD from 6 cities across India with cough as the chief complaint. The survey was conducted over a period of 3 months, from October to December 2017. The It collected demographic details, duration of cough, history of similar episodes in past 12 months, nature, intensity and frequency of cough, associated symptoms, co-morbid conditions, concomitant medications, history of self-medication, adverse effects due to self-medications, classes and duration of drugs prescribed for cough and patient preference for treatment. Intensity of cough was categorized into 3 types; fairly intense (Tiresome, but is able to continue routine), low in intensity (Comfortably carries out routine) and high intensity (Routine life interrupted). Approximately 10 children were enrolled from each site and 250 to 300 from a region.
Statistical analysis
No formal sample size calculation was performed being non-interventional nature of the study. Only standard descriptive statistics is reported in the results. No comparative statistical analysis is performed. Categorical data are presented as percentages.
Results
A total of1998children (58% males; 41% females, 1% not mentioned)were enrolled from 6 cities namely Bangalore (350), Ahmedabad (249), Delhi (403), Hyderabad (298), Lucknow (397) and Mumbai (301).
Age group-wise distribution
Majority (40 %) of children enrolled in this survey belonged to 3-6 years of age (Figure 1). While 1-8 years old comprised 75% of children surveyed.
Duration of Cough
68% children had cough symptoms since 5 days prior to OPD visit while 3% children had symptoms forover 10 days (Figure 2).
History of similar cough episodes
A total of 46% of the childrenhad 4-6 similar episodes of cough symptom in the preceding 12 months (Figure 3).
Nature of cough
A total of 61% of the children had productive cough while 25 % had dry cough with no or minimal sputum (Figure 4).
Intensity of cough
67% of the children hadfairly intense symptoms but were able to continue their routine activities while 15% had cough symptoms severe enough to affect their routine life such as -attending school/ kindergarten (Figure 5).
Number of cough bouts per day
37% children reported 2-6 cough bouts per day. More than half of the children had more than 6 bouts and 21% reported more than20 cough bouts per day (Figure 6).
Associated symptoms
Fever (63%) was the most commonly reported associated symptom with their current cough episode. Other reported symptoms included running nose (53%), sore throat or throat pain (45%), nasal stuffiness (43%), sneezing (40%), headache (39%), sleep disturbance (including snoring) (37%), breathlessness (31%), hoarseness of voice (29%) and nasal irritation or itching (22%). 3% of the children also had fatigue, body ache and skin rashes during the cough episodes (Figure 7).
Presence of risk factors for precipitation of cough
Associated risk factors for precipitating present cough episode were conditioned/cold air (1%), intake of cold drinks (1%) and chilled water (2%); asthma (2%), malnutrition/ nutritional deficiency (4%) and season/ weather change (7%),reported in less than 10% of children. Exposure to smoking / pollution at home or school (23%), known or suspected immune deficiency (19%) and allergic rhinitis (15%) were quite frequently associated for their current cough episode. 28% respondents were unaware about anyriskfactorassociated for their current cough episode (Figure 8).
Concomitant medication
22% of the children were taking concomitant medications while remaining majority (78%) were not taking any other medication.
Practice of Self-medication
Although majority (74%) of children had no history of self-medication reported, 26% children were self-medicated for present or in past cough episode(s).
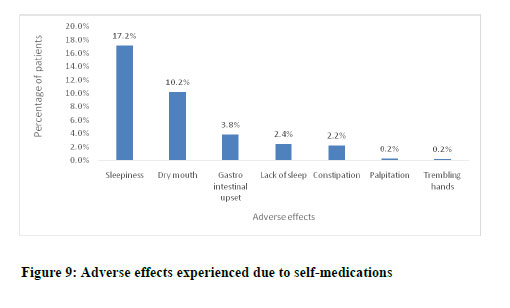
Adverse effects due to self-medication
Sleepiness was the most common adverse effect reported due to self-medication (45%; n=343). Dry mouth 29% (222), gastro intestinal upset 10% (80), lack of sleep 6%(49) and constipation in 7% (57)were other adverse effects reported due to self-medication(Figure 9).
Preference of Formulation
Syrup was preferred by 61% children whereas 13% preferred tablets by grown-up children.
Type of Medications Prescribed for Current Symptoms
78% children received first generation sedative antihistamines while 76% were prescribed second generation non-sedative antihistamines. Antibiotics (50%) and nutritional supplements (12% ) were prescribed besides mucolytics (62%) and expectorants (63%) (Table 1). 78% of children were prescribed with antitussives (61% dextromethorphan, 13% codeine). Majority of cases were prescribed antitussives up to 6 days (Figure 10).
Just 3% of children were prescribed with corticosteroids in the form of nasal spray. 80% of these children were prescribed for just 1-3 days while rest were advised up to 6 days. (Table 1) Oral route was preferred in majority (83%) of cases (Figure 11).
Discussion
In this cross sectional questionnaire based survey across the country, children presenting with cough were screened and evaluated for different parameters. The survey provides information on important aspects like duration and type of cough, presence of risk factors, self-medicationif anyand associated adverse effectsof drugs on children. The survey was conducted with help of 200 pediatricians from 6 cities across India.
Childhood acute respiratory infection (ARI) is a significant public health problem, especially in developing countries. In an Indian study22 on 397 school children in age group of 5-14 years, 52% of children presenting with acute respiratory infection (ARI) belonged to 5-9 years age group. In our survey, 40% children belonged to 3-6 years age group.An observational study by De Blasio et al7 also reported almost half of the children presenting acute cough in 1-5 year age-group. Children in this age group have various habits that promote easy transmission of infections.As such this is the age when children are introduced to out-of-home careand thus susceptible to infections because of lack of previous exposure to common infective organisms. Besides, there are physiological reasons like the immature immune system and dysfunctional eustachian tube predisposing them to upper airway infections17. Our present study affirms the fact that preschool and nursery age group children are more prone to infections than others.
Classification of cough based on the duration relies on available data related to URTI in children. Cough may continue for 10-25 days in children with common cold or viral respiratory tract infections2.British Thoracic Society (BTS) guidelines defined acute cough as a recent onset of cough lasting less than 3 weeks21. Different guidelines label chronic cough as ranging from 3-12 weeks. 68% children in this survey had cough up to 5 days prior to their presentation to the OPD. 95% children in this survey can be considered as cases of acute cough since the duration of presentation of cough was less than 10 days. Children in an observational study7 showed mean duration of acute cough to be around 4-5 days, ranging from 2 to 21 days.
Acute respiratory infections usually produce 5 to 8 episodes of cough in a year in children; each lasting for 7 to 9 days. 45% Children in our survey reported 4 to 6 similar episodes of cough in preceding 12 months, suggesting underlying athma or virus induced tracheo-bronchial hyper-reactivity states, more in winter months during which the study was conducted, that too, in the metropolitan cities where the pollution level is much higher.
Cough is usually categorised based on duration of cough rather than frequency. As such, two or more episodes of cough, without any history of viral URI (Coryxa, cough and cold) in past one year considered as recurrent cough. However, recurrent cough in short intervals, even with resolutions, cannot be easily differentiated from persistent chronic cough18. Thus, recurrent cough episodes seem to be quite prevalent in children in our country.
Childrenwith cough is usually heterogenous, with varied risk factors and comorbid conditions3. Our study population was heterogenous in terms of age group and type of cough. Contrary to usual belief, wet and productive cough was commonly observed in our survey(61%) than dry 25% and bronchospastic cough (14%; n=270).Previous survey conducted by Narayanan et al16reported dry cough (57%) more commonly than productive (40%) and bronchospastic (3%) cough. De Blasio et al reported dry cough as more common in their observational study in 433 children7. While the Indian study study16 included majorly adult population, our survey was pediatric age specific under 12 years of age. However, there could be other factors in operation, leading to such differences. Environmental factors are supposed to affect the transmission of viral respiratory infections19. The survey by Narayanan16 was conducted in two different seasons, our present survey was mostly limited to winter season only when viral (RSV and others) infections are so common, with immune mediated cough. These aspects can be the reason for the observed variation. Despite these findings, the use of antitussives such as – dextromethorphan and codeine was found to be more prevalent (74%;n=1480)in our study.There is a need to understand that viral ARI always not confined to dry cough. Very often than not, the involvement of tracheo bronchial tree with immune mediated mucosal oedema, sticky secretions result in spasmodic and paroxysmal cough in a vicious cycle of vagal timulation, not amounting to active broncospasm as in asthma. Higher incidence of wet and productve cough in our study conducted during inter months, may be atributable for this patho-physiology. Antitussives, particularly opioids are certainly not desirable. Plenty of fluid intake, frequent saline nose drops, a mild second generation decongestant are good enough with or without a short course of bronchodilator if at all, in moderate to severe extent of cough. Steroids have no role to play.
De Blasio et al7 assessed the intensity of cough as mild, moderate and severe. Wide variation in intensity of cough from low to fairly intense severity was seen in our study, with moderate intensity being more common (58%). Although mild to moderate cough or low to fairly intense cough maynot interfere with daily routine, parents might refrain from sending these kids to school, especially if associated with fever, to avoid increase in severity of symptoms as well as prevent spread of infection to other classmates. Cough and cold lead to missed school days for children which ultimately force missed office days for working parents who need to stay at home to care for children1.
Majority of children in our survey had more than 6 cough bouts per day. 21% children were having even more than 20 cough bouts per day. This can be the reason for early consultation with pediatricians seen in the survey. The previous survey16 also reported similar results (More than 6 bouts-56%; More than 20 bouts-17%).
Children in our studyreported different symptoms including fever, running nose, sore throat or throat pain, nasal stuffiness, sneezing, headache, sleep disturbance (including snoring), breathlessness, hoarseness of voice and nasal irritation or itching. Most of these symptoms are commonly seen with viral respiratory illnesses. Fever, cough and rhinorrhea are the most common symptoms seen with acute respiratory infections and were correspondingly frequent in our study population (fever 63%, rhinorrhea 53%)3. However, Suguna et al22reported fever in 13.6% of school children with acute respiratory infections. Previous survey, majorly comprising of adults, by Narayanan et also reported less frequent fever (12%).
There are several risk factors known to precipitate cough. Potts et al20 assessed indoor risk factors for cough and found that tobacco smoke, poor ventilation, coal as cooking fuel, mold and dampness as important contributors. Association of malnutrition, younger age, low coverage of immunization, early childhood mismanagement and respiratory damage has been found to be significant risk factors in development of respiratory illness like pneumonia8. In the 5-9 years age group, family history of allergic disorder and asthma, presence of smoke outlet in kitchen, absence of windows in sleeping room are also found to have an independent association with the ARI. In our survey, exposure to smoking or pollution at home or school, known or suspected immune-deficiency and allergic rhinitis were identified as associated risk factors for coughin many children.
Although the effects of cough and cold are temporary, its high prevalence has remarkable bearing on quality of life and economic burden. The typical commoncold management is usually through useof antihistamines, antitussives, mucolytics anddecongestants.Many consumers are aware of risk of drug interactions of prescribed drug for other comorbid conditions and OTC cough and cold medicines11. Fewer children (22%) in our survey were on concomitant medication leading to decreased chances of drug interaction with cough medication. The practice of self-medication was reported to be less (26%) in the surveyed population which is quite high. A study conducted by Ahmad et al to evaluate self-medication practice in India found that 11.7% of the study population was taking self-medication for respiratory disease. Among the self-medications, use of cough syrup containing antihistamineswas common in our study.Sleepiness (45%)was the most common adverse event associated with self-medication followed by dry mouth (29%) which are well-known side effects of anti-histamines, especially first generation agents.
First generation 78% (1560) and second generation 76% (1520) usage of antihistaminics werefound to be high. The data also reflects thatsome of thechildren were given both generation antihistaminic drugs together. Although, both first- and second-generation antihistamines are blockers ofH1-receptor sites, there is an additional pharmacological activity of the first-generation antihistamines as the competitive antagonism of acetylcholine at neuronal and neuromuscular muscarinic receptors. The effectiveness of first-generation antihistamines in reducing sneezing in colds is supposed to be due to neuro-pharmacological manipulation of histaminic and muscarinic receptors in the medulla15. That is why,the first-generation antihistamines are commonly used in cough formulations for prompt relief. But the resulting drowsiness, sticky secretions on bronchial mucosa are counter productive. As the individual tries to dislodge these dried secretion inducind cough, the reound vagus stimulation induces a vicious cycle of more and more cough and broncho spasm. The American Academy of Paediatrics stated that OTC medicines are generally safe only if used as per product labelling. AAP raised concerns on chances of increased risk of adverse effects due to usage of multiple multi-ingredient preparations having same active ingredient. Inappropriate dosing of cough and cold medications is another important concern12. The cross sectional studyt reported 37% prevalence ofmultiple antihistaminesuse for upper respiratory infection in children less than 6 years of age. Practice of prescribing multiple histamines as reported in that study as well seen in the current survey pose a risk of increased adverse effects on children.
Acute respiratory infections are commonly associated with low-grade fever.The symptoms and signs of the common cold start with nasal stuffiness and throat irritation, usually accompanied by low-grade fever, anorexia and myalgia. Sneezing is associated with a watery nasal discharge, which becomes mucopurulent in 1 to 3 days; can persist for up to 10 days in many. Cough occurs probably due to inflammation of the lower respiratory tract5. Antipyretic use was found common (69%)corresponding with high number of childrenwith fever (63%) in our survey.Antibiotic use in childhood URTIs has always been an issue since more than 90% of suchinfections are of viral aetiology5. The same is highlighted in our study with half of the children being prescribed antibiotics albeit for short duration (3 to 6 days) in the majority prescribed.Short courses of decongestants were also commonly seen in 42% of children.
Despite greater number of children reported with wet and productive cough,albeit with scanty expectoration, use of antitussives was paradoxically higher (74%) in our study. This shows wide variation from management protocols and guidelines in clinical practice. Use of dextromethorphan was found to be more common as compared to codeine which is in line with its expected advantages7.
More than half of ourchildren preferred syrup over tablet which was quite obvious considering the surveyed age group. The preference can be attributed to swallowing ease and soothing effect of syrupsin younger children.
The current survey provides significant insights into patient profile of acute cough among children and its management. Large sample size andenrolment of patients from different regions of the country are the strengths of this study.
Conclusion:
Acuteonset and recurrent nature of cough isa common observation in pediatric age group. Exposure to environmental pollutants both at home and schoolseems to bean important risk factor.Cough in children is often associated with expectoration or sputum production, albeit scanty, contrary to our belief. Grown-up children are able to bring out sputum better while younger ones usually swallow it down, Fever, runny nose and sore throat are the most commonly associated symptomsalong with pediatric cough. Decongestants, antitussives, opioids, antihistamines, expectorants and mucolytics are commonly prescribed by pediatricians for management of cough in children, not always as per guidelines.Prescription of multiple antihistamines needs to be discouraged and awareness is required in treating physicians about risk of drug toxicities when prescribing multiple multi-combination preparations. Self-medication may be harmful for children about which public awareness drives are welcome.
Role of Authors:
Dr H. Paramesh: Concept and study design, Dr. N. C. Mohanty: Study design, Data interpretation, manuscript writing, Dr. V.Kamale: Data analysis and final editing, Dr. V. Patra: Monitoring data collection, first editing, Dr. R. Jain: Dr. R. Jain: Administration, supervision and manuscript writing, Dr. G. Pappulwar: Co-ordination between study centres and manuscript writing, Dr. R. Rathod: Data collection, Tables, figures and manuscript writing.
Conflict of Interest: None
Acknowledgments
We would like to acknowledge M/S Wockhardt Ltd and Empulse Research, Data Analytics (I) Pvt Ltd for providing technical and logistic while carrying out this survey.
Reference:
1. Allen LV. Colds & cough. Int J Pharm Compd. 2012 Nov-Dec;16(6):480-3.
2. Alsubaie H, Al-Shamrani A, Alharbi AS, Alhaider S. Clinical practice guidelines: Approach to cough in children: The official statement endorsed by the Saudi Pediatric Pulmonology Association (SPPA). Int J Pediatr Adolesc Med. 2015 Mar;2(1):38-43.
3. Budge PJ, Griffin MR, Edwards KM, Williams JV, Verastegui H, Hartinger SM, et al. A household-based study of acute viral respiratory illnesses in Andean children. Pediatr Infect Dis J 2014;33:443-7.
4. Cornford CS, Morgan M, Ridsdale L. Why do mothers consult when their children cough? Fam Pract 1993;10:193-6.
5. Cotton MF, Innes S, Jaspan H, Maddie A, Rabie H. Management of upper respiratory tract infections in children. S Afr Fam Pract (2004).2008;50(2):6-12.
6. De Blasio F, Dicpinigaitis PV, Rubin BK, Danieli GD, Lanata L, Zanasi A. An observational study on cough in children: epidemiology, impact on quality of sleep and treatment outcome. Cough 2012;8:1. As available online at https://doi.org/10.1186/1745-9974-8-1
7. De Blasio F, Virchow JC, Polverino M, Zanasi A, Behrakis PK, Kilinç G et al. Cough management: a practical approach. Cough. 2011;7:7. doi: 10.1186/1745-9974-7-7
8. Fatmi Z, White F. A comparison of ‘cough and cold’ and pneumonia: risk factors for pneumonia in children under 5 years revisited. Int J Infect Dis 2002; 6: 294-301.
9. Kai J. What worries parents when their preschool children are acutely ill, and why: a qualitative study. BMJ 1996;313:983-6.
10. Kaushik A. Formulation and evaluation of herbal cough syrup. Eur J Pharm Med Res 2016;3(5):517-522.
11. Kloosterboer SM, McGuire T, Deckx L, Moses G, Verheij T, Driel M. Self-medication for cough and the common cold: information needs of consumers. Aust Fam Physician. 2015 Jul;44(7):497-501.
12. Lui CT. Prescription practice of antihistamines for acute upper respiratory tract infections in pediatric patients in a local emergency department in Hong Kong. World J Emerg Med. 2017;8(1):47-54.
13. Mahashur A. Chronic dry cough: Diagnostic and management approaches. Lung India. 2015 Jan-Feb; 32(1): 44-49.
14. McKenzie S. Cough – but is it asthma? Arch Dis Child 1994;70:1-2.
15. Muether PS. Gwaltney JM. Variant Effect of First- and Second-Generation Antihistamines as Clues to Their Mechanism of Action on the Sneeze Reflex in the Common Cold. Clinical Infectious Diseases 2001;33(9):1483-8.
16. Narayanan V, Pawar S, Rege P. Patient Profile and Prevailing Trends of Cough Management in India: Results of the COFPRO Survey. Cough Management Study. The Indian Practitioner 2017;70(10):17-24.
17. Nesti M, Goldbaum M. Infectious diseases and daycare and preschool education. J. Pediatr (Rio J). 2007;83(4):229-312.
18. Ng MCW, How CH. Recurrent wheeze and cough in young children: is it asthma? Singapore Med J. 2014 May; 55(5): 236-241.
19. Pica N, Bouvier NM. Environmental Factors Affecting the Transmission of Respiratory Viruses. Curr Opin Virol. 2012 Feb; 2(1): 90-95.
20. Potts JF, Rona RJ, Oyarzun MJ, Amigo H, Bustos P. Indoor Risk Factors for Cough and Their Relation to Wheeze and Sensitization in Chilean Young Adults. Am J Public Health. 2008 April; 98(4): 680-686.
21. Shields MD, Bush A, Everard ML, McKenzie S, Primhak R; British Thoracic Society Cough Guideline Group.BTS guidelines: Recommendations for the assessment and management of cough in children.Thorax. 2008 Apr;63 Suppl 3:iii1-iii15.
22. Suguna E, Kumar S G, Roy G. Prevalence and risk factors of acute respiratory infection among school children in coastal South India. J Global Infect Dis 2014;6:95-8
23. Thomson F, Masters IB, Chang AB. Persistent cough in children and the overuse of medications. J Paediatr Child Health 2002;38:578-81.
24. Worrall G. Acute cough in children. Can Fam Physician. 2011 Mar; 57(3): 315-3182
Issue: January-March 2019 [Volume 8.1]